Yes, COVID19 can set off a flare of reactive arthritis, usually showing up 14 weeks after the virus clears, with joint pain, swelling, and stiffness that most people see improve in weeks to a few months.
Most cases are mild and respond to over-the-counter anti-inflammatories, but it's still worth getting checked out to rule out other rheumatic conditions and to make sure you're not missing anything seriousespecially if you're worried about the vaccine or long-COVID joint aches.
Why People Ask
Is it real?
People wonder whether reactive arthritis COVID is just internet hype or a genuine medical phenomenon. The answer is a solid yes. Several peer-reviewed studies, including a 2024 case series in BMJ Case Reports, have documented patients developing joint inflammation shortly after a confirmed COVID19 infection.
How long does it last?
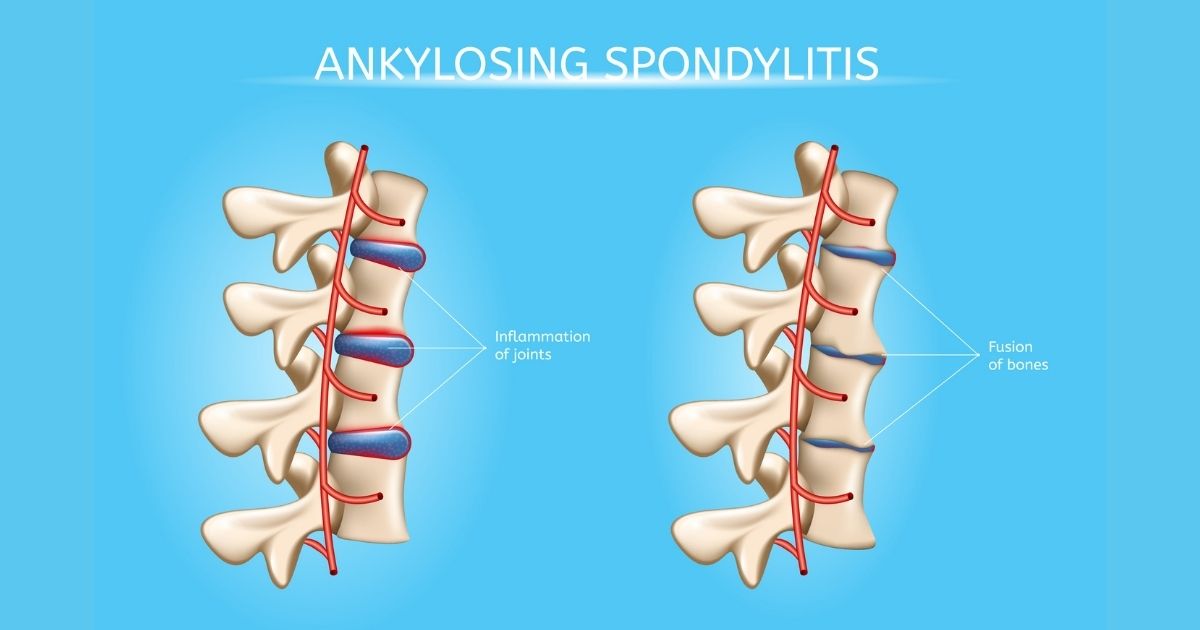
Most folks report that symptoms subside within three to six months, but about 1015% may need longer treatment, especially if they have a genetic predisposition like HLA-B27. Understanding the ankylosing spondylitis criteria can sometimes help doctors distinguish between reactive arthritis and underlying spondyloarthritis conditions if symptoms linger.
Is the vaccine responsible?
Reports of reactive arthritis after the COVID19 vaccine are extremely rareroughly 1 in 100,000 casesand the benefits of vaccination far outweigh that tiny risk. A review in Rheumatology Advisor concluded the vaccine-related risk is negligible compared with the joint problems that can follow an actual infection.
The Science Behind
What is reactive arthritis?
Reactive arthritis is an immune-mediated inflammation that strikes joints, tendons, and sometimes eyes or the urinary tract, without the bacteria or virus actually being in the joint. Think of it as the body's overenthusiastic alarm system that keeps ringing after the invader has left.
How COVID triggers it
Direct viral mechanisms
Studies have found fragments of the SARS-CoV-2 spike protein lingering in synovial tissue, sparking a local immune response. This direct viral theory explains why some patients develop arthritis even when the virus is no longer detectable in the bloodstream.
Molecular mimicry
COVID19 can also confuse the immune system: some viral proteins look suspiciously like proteins found in joint linings. The immune system attacks both, a phenomenon called molecular mimicry. This mechanism is supported by cytokine storm data showing high IL6 and TNF levels in the weeks after infection.
Is it the same as Long COVID arthritis?
Not exactly. Long COVID arthritis usually refers to lingering joint pain that can be more diffuse and noninflammatory, while reactive arthritis is a defined, inflammatory reaction that often follows a pattern (knees, ankles, heels). Both can coexist, but they're distinct entities.
Vaccine-related cases
When a handful of patients report joint swelling after a shot, researchers look for a temporal link. The consensus in the medical community is that the spike protein generated by mRNA vaccines is far less likely to cause the same tissue-level persistence seen after a natural infection. In short: the vaccine's safety profile remains rock solid.
Spotting the Symptoms
Classic signs
Typical reactive arthritis symptoms include:
- Sudden joint pain and swelling, most often in the knee, ankle, or foot.
- Stiffness that's worse in the morning but improves with movement.
- Enthesitistenderness where tendons attach to bone, especially the heel. This is also seen in ankylosing spondylitis shoulder pain and related spondyloarthropathies.
- Occasional eye redness (conjunctivitis) or urinary discomfort, though these aren't always present.
Typical timeline
After a COVID19 diagnosis, the joint flare usually emerges between 7 and 28 days. The first sign many Reddit users share on reactive arthritis covid reddit threads is an achy ankle that feels "off" after they've already recovered from the respiratory symptoms.
Real-world example
Consider Maya, a 32-year-old teacher who had a mild bout of COVID19 in March. Ten days after testing negative, she noticed swelling around her left ankle and a stiff knee that made walking to the kitchen a chore. After trying ibuprofen for a few days with modest relief, she visited her rheumatologist, who confirmed reactive arthritis and prescribed a short course of NSAIDs. Within three weeks, Maya's pain had faded enough to jog with her kids again.
How Doctors Diagnose
Clinical evaluation
Physicians start with a focused history: recent COVID infection, symptom onset, and any extra-articular clues (eye irritation, urinary symptoms). A physical exam then checks for asymmetric joint swelling and enthesitis.
Lab & imaging tests
Typical lab findings include elevated ESR or CRP, negative rheumatoid factor, and sometimes a positive HLA-B27 test. X-rays usually look normal early on, while an ultrasound can reveal joint effusion and tendon insertion inflammation.
Diagnostic flowchart
| Step | Action |
|---|---|
| 1 | Confirm recent COVID19 infection (PCR or antigen test). |
| 2 | Document joint pain pattern and extra-articular signs. |
| 3 | Order ESR/CRP, rheumatoid factor, HLA-B27. |
| 4 | Perform ultrasound or X-ray if needed. |
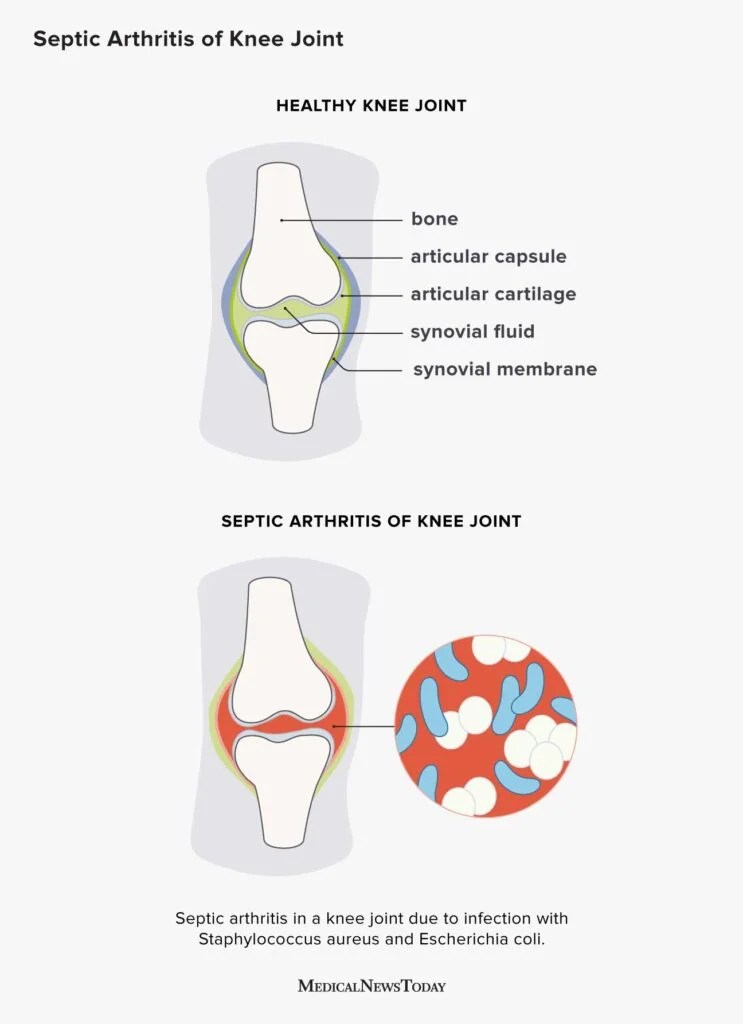
| 5 | Rule out septic arthritis and other rheumatic diseases. |
| 6 | Diagnose reactive arthritis if labs support inflammation and infection timeline fits. |
Effective Treatment Options
First-line NSAIDs
Over-the-counter NSAIDs such as ibuprofen or naproxen are the go-to. They reduce inflammation and give pain relief within a few hours. For most people, a two-week course at the recommended dose is enough, followed by a taper if symptoms improve.
When to step up
If pain persists beyond three weeks or joints become very swollen, doctors may prescribe a short tapering course of oral corticosteroids. For chronic or recurrent cases, disease-modifying antirheumatic drugs (DMARDs) like sulfasalazine or methotrexate are considered.
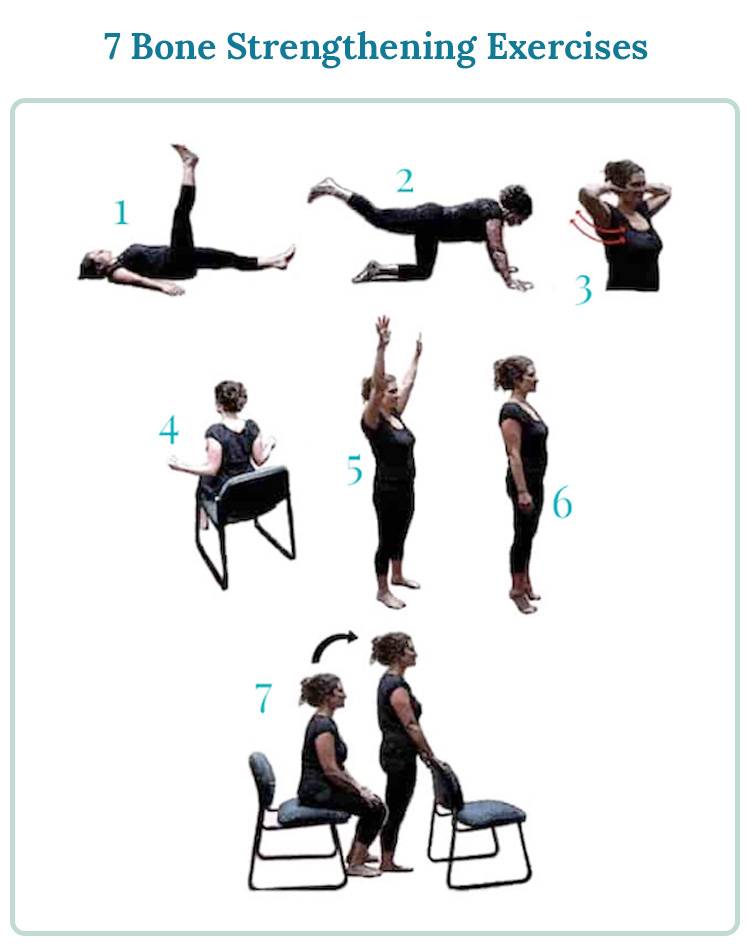
Physical therapy tips
Gentle range-of-motion exercises keep joints supple without aggravating inflammation. A simple routine includes ankle circles, heel raises, and knee extensions performed twice daily. If you're experiencing persistent hand swelling or musculoskeletal symptoms, a look at hand swelling advice can be useful for differentiating between arthritic and other causes.
Maintaining a healthy weight also eases joint stress.
Managing flare-ups
When a flare strikes, try:
- Ice packs on the affected joint for 1520 minutes.
- Elevating the limb to reduce swelling.
- Resting the joint, but avoiding complete immobilization.
- Resuming NSAIDs at the lowest effective dose.
Many Reddit contributors share success with a combo of ibuprofen, ice, and a short walk to keep synovial fluid moving.
Bottom Line Summary
Reactive arthritis after COVID19 is a genuine, albeit uncommon, post-infectious condition that typically appears within a month of the virus and often resolves with simple anti-inflammatory treatment. While isolated reports link the COVID19 vaccine to similar joint aches, the risk is minuscule compared with the protective benefits of vaccination. Recognizing the classic symptom pattern, seeking timely medical evaluation, and following a stepwise treatment plan can keep you back on your feet without unnecessary worry.
If you've experienced sudden joint pain after a COVID infection or vaccination, don't ignore ittalk to a rheumatologist. Early care can turn a frustrating flare into a brief, manageable episode. And remember, you're not alone; many people have walked this path and found relief. Stay curious, stay informed, and take care of those jointsyou deserve to move freely and comfortably.
FAQs
Can COVID‑19 trigger reactive arthritis?
Yes. SARS‑CoV‑2 can ignite an immune‑mediated joint inflammation that typically appears 1–4 weeks after the infection clears.
What joints are most commonly affected?
The knees, ankles, and heels are the usual sites, often presenting with swelling, pain, and enthesitis at tendon insertions.
How is reactive arthritis after COVID diagnosed?
Doctors look for a recent COVID infection, asymmetric joint swelling, elevated ESR/CRP, negative rheumatoid factor, and may order an HLA‑B27 test and joint ultrasound.
Are NSAIDs enough for treatment?
For most people, over‑the‑counter NSAIDs such as ibuprofen or naproxen relieve symptoms within a few weeks; steroids or DMARDs are reserved for persistent cases.
Is the COVID‑19 vaccine a risk factor?
Vaccine‑related reactive arthritis is exceedingly rare (≈1 in 100,000) and far outweighed by the protective benefits of vaccination.