Quick Answer
If youre wondering what the most common junctional rhythm symptoms are, heres the short version: you may feelfatigue, dizziness, lightheadedness, occasional palpitations, or even a brief fainting spell. In many cases the rhythm is quiet and you wont notice anything at allyour doctor might catch it on a routine ECG. When symptoms are present, they usually signal that the hearts normal pacing system needs a little extra attention.
Understanding Junctional Rhythm
What is a junctional rhythm?
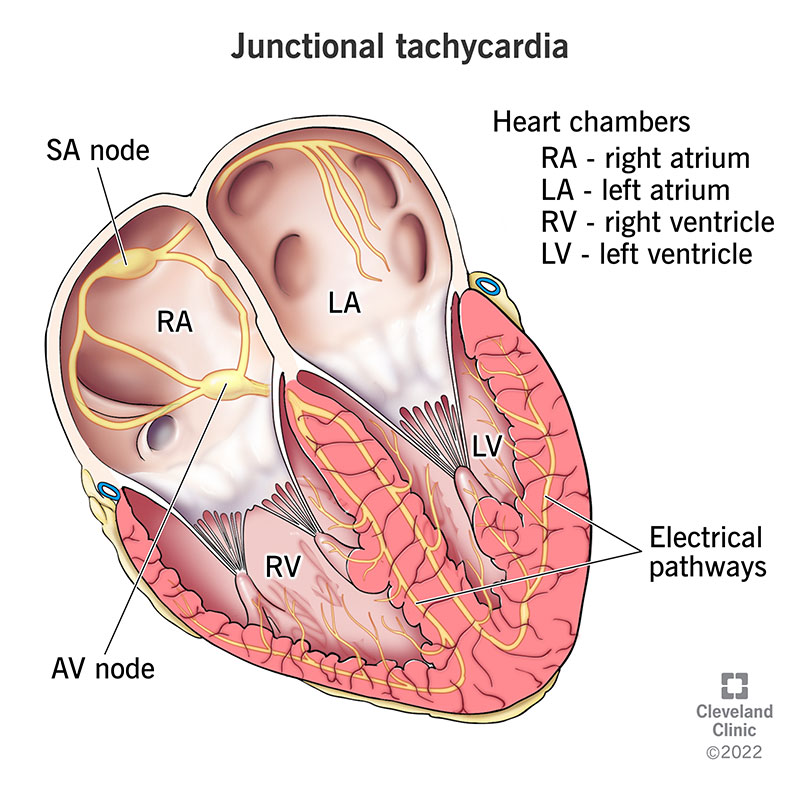
Think of your heart as a wellorchestrated band. The SA node is the lead singer, setting the tempo. When the singer goes offkey or takes a break, the AV node (the junction) can step up and keep the music playing. That backup beat is what we call a junctional rhythm. Its still a regular rhythm, just generated a few beats lower in the conduction pathway.
Rhythm Types at a Glance
| Rhythm type | Typical heart rate (bpm) | ECG hallmark | Common trigger |
|---|---|---|---|
| Junctional escape rhythm | 4060 | Absent or retrograde Pwaves, narrow QRS | SAnode failure |
| Accelerated junctional rhythm | 60100 | Same as escape but faster | Digoxin toxicity, myocardial infarction |
| Junctional tachycardia | >100 | Regular narrow QRS, no upright Pwaves | Digitalis overdose, ischemia |
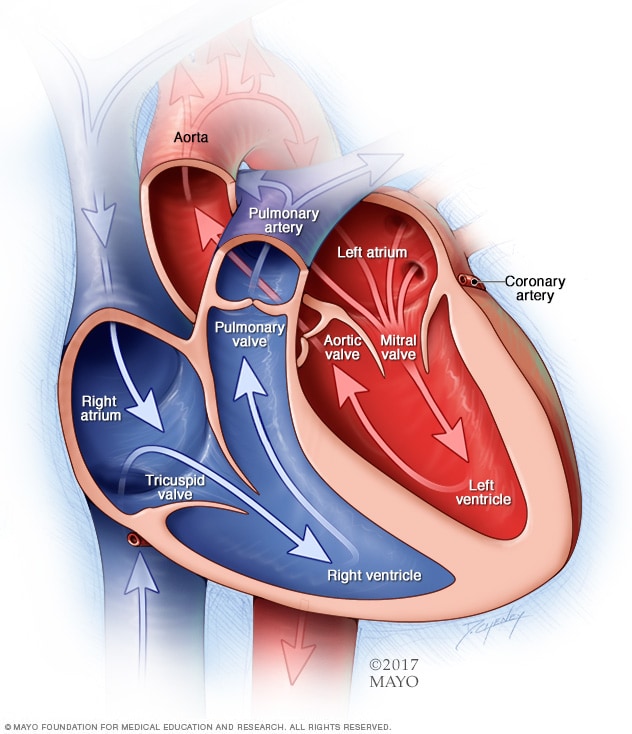
How does the hearts electrical system work?
The hearts electrical highway starts at the SA node (the natural pacemaker), travels through the atria, pauses at the AV node, and then races down the HisPurkinje system to make the ventricles contract. If the SA node falters, the AV node can fire on its ownthis is the junctional escape that keeps blood moving. Its a clever safety net, but it can also produce those patterns youll see later.
Core Symptoms
Most common junctional rhythm symptoms
Everyones experience is a little different, but the following tend to show up most often:
- Fatigue or low energy like youve been running on a drained phone battery.
- Dizziness or lightheadedness the room may feel a bit spun when you stand up.
- Syncope or nearsyncope a brief blackout or the sensation of about to faint.
- Palpitations a flutter or thump that you can actually feel in your chest.
- Shortness of breath especially during a climb up stairs or a gentle jog.
Realworld anecdote
One of my patients, Sam, thought his headspin was just stress from work. He finally went to his doctor after a fainting episode while reaching for a coffee mug. The ECG showed a junctional escape rhythm, and adjusting his medication cleared the symptoms within a week. Stories like Sams remind us how easy it is to dismiss subtle clues.
When you might feel fine
Its not all drama. Some people live with a junctional rhythm and never notice a thing. Often the rhythm is discovered incidentally during a routine checkup or preop assessment. In those cases the heart is simply doing its job quietly, and no urgent intervention is needed.
Why Does It Happen?
Primary causes of junctional rhythm
There are several usual suspects that can push the hearts pacing up to the AV node:
- SAnode failure agerelated fibrosis or sicksinus syndrome.
- Medication effects digoxin toxicity, highdose betablockers, or calciumchannel blockers.
- Ischemic heart disease a heart attack that damages the SA node.
- Electrolyte disturbances especially high potassium (hyperkalemia).
- Postoperative changes after cardiac surgery or ablation procedures.
Cause vs. Rhythm Table
| Cause | Likely rhythm outcome | Typical symptoms |
|---|---|---|
| SAnode disease | Junctional escape rhythm | Fatigue, bradycardia |
| Digoxin toxicity | Accelerated junctional rhythm | Palpitations, nausea |
| Inferiorwall MI | Junctional tachycardia | Chest pain, dyspnea |
| Hypoxia | Junctional escape rhythm | Lightheadedness |
Secondary or rare triggers
Less common culprits include hypothyroidism, autonomic dysfunction, and even severe infections that stress the heart. While theyre not the headline causes, they can still tip the balance toward a junctional rhythm, especially in vulnerable individuals.
Diagnosis: Reading the ECG
Key ECG features of junctional rhythm
The junctional rhythm ECG has a few signature clues:
- No upright Pwaves before the QRS complex (they may appear after the QRS or be hidden).
- Regular, narrow QRS complexes.
- Heart rate that tells you which subtype youre staring at (see the earlier table).
ECG Image Placeholder (alt text suggestion)
Imagine a strip where the spikes (QRS) march steadily, but the little P blips are either missing or tucked in after each spike. Alttext could read: ECG showing regular narrow QRS complexes with hidden or retrograde Pwaves, indicating a junctional escape rhythm.
When to order further tests
If the rhythm is intermittent, if youre unsure about the cause, or if symptoms are severe, doctors often add:
- Holter monitoring (2448hr recording).
- Event monitor for sporadic episodes.
- Blood work for electrolytes, thyroid function, and digoxin levels.
- Stress testing if ischemia is suspected. For example, an exercise stress test can help reveal ischemia that might be triggering junctional rhythms.
Is a Junctional Rhythm Dangerous?
When it isnt a major threat
Many people live happily with a stable junctional escape rhythm ranging from 4060bpm. If you feel fine and your doctor sees no underlying problem, the best treatment may be simple observation.
When it can be risky
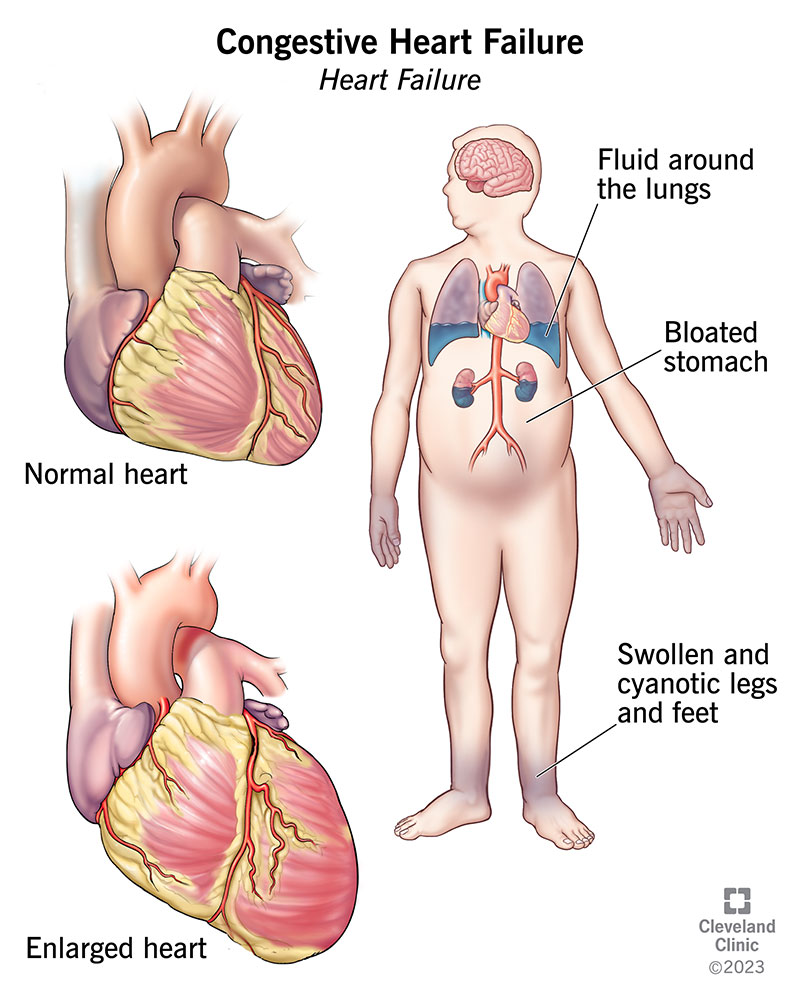
Danger usually creeps in when the heart rate drops too low, climbs too fast, or the rhythm is a sign of something else (like a heart attack). In those scenarios the rhythm can cause:
- Reduced blood flow to the brain fainting.
- Worsening heart failure symptoms.
- Misinterpretation of atrial arrhythmias, leading to inappropriate medication.
Redflag checklist
| Symptom | Why it matters | What to do |
|---|---|---|
| Fainting (syncope) | Possible cerebral hypoperfusion | Seek emergency care immediately |
| Chest pain or severe shortness of breath | May indicate myocardial infarction | Call EMS |
| Heart rate<40bpm with dizziness | Significant bradycardia | Contact your cardiologist promptly |
Treatment Options
Initial treatment for junctional rhythm
The first step is always to look for reversible causes. That means:
- Stopping or adjusting any medication that might suppress the SA node.
- Correcting electrolyte imbalances (like high potassium).
- Treating underlying hypoxia or thyroid issues.
- Monitoring the patient closely if symptoms are mild.
Decisiontree flowchart (description)
Picture this: You start at Patient presents with junctional rhythm. If asymptomatic Observe, repeat ECG in 612months. If symptomatic Check vitals, labs, meds. If bradycardic <40bpm Consider atropine or temporary pacing. If rapid >100bpm Assess for digoxin toxicity, consider blocker.
Specific therapies
When the rhythm needs more than observation, treatments can include:
- Pharmacologic: Atropine for acute bradycardia, isoproterenol for accelerated rhythms.
- Device therapy: Permanent pacemaker implantation if the junctional rhythm is persistent and symptomatic.
- Lifestyle tweaks: Staying hydrated, avoiding excessive alcohol, and regular followup ECGs.
Accelerated junctional rhythm treatment
If the hearts beating faster than the usual escape rate, the culprit is often medicationrelated (digoxin) or ischemia. The typical approach:
- Reduce or stop the offending drug (e.g., lower digoxin dose).
- Treat underlying ischemia if present maybe a coronary angiography.
- If the rate stays above 100bpm, a lowdose blocker or calciumchannel blocker can calm things down.
Guidelines from the recommend close monitoring during any medication adjustment.
Practical Takeaways
Selfmonitoring checklist
Being proactive can make a huge difference. Keep a simple log:
- Heart rate (bpm) you can use a smartwatch or manually check pulse.
- Time of day symptoms appear.
- Recent medication changes or new supplements.
- Any accompanying feeling (dizziness, chest tightness, etc.).
Review this with your doctor at each visit. It helps spot patterns that a single ECG might miss.
Downloadable symptomlog (suggested)
Consider offering readers a printable PDF table they can fill out at home. A short note says: Track your hearts rhythm and symptoms knowledge is power.
When to schedule followup appointments
Mark your calendar for a checkup:
- Within 12weeks after any medication change.
- If you experience new or worsening symptoms.
- After any emergency department visit for syncope or chest pain.
- Every 612months for routine surveillance if you have a known junctional rhythm.
Wrapping It Up
Bottom line: junctional rhythm symptoms can range from a silent, harmless background beat to a warning sign that something needs attention. Recognizing the key signsfatigue, dizziness, fainting, or palpitationshelps you act quickly. Diagnosis is straightforward with a standard ECG, and treatment is often as simple as fixing reversible causes or, in more serious cases, using medication or a pacemaker. By staying informed, monitoring your own rhythm, and keeping an open line with your healthcare team, you can keep your hearts backup singer from stealing the show. If youve experienced any of these symptoms, share your story in the comments or reach out to a cardiology specialistyour experience might help someone else feel less alone.
FAQs
What are the most common junctional rhythm symptoms?
Typical signs are fatigue, dizziness or light‑headedness, occasional palpitations, shortness of breath, and in some cases fainting (syncope) or near‑syncope.
Can a junctional rhythm be asymptomatic?
Yes. Many people have a junctional rhythm that causes no noticeable symptoms and is discovered incidentally on a routine ECG.
How is a junctional rhythm diagnosed on an ECG?
Key ECG clues include regular narrow QRS complexes, absent or retrograde P‑waves (often hidden or occurring after the QRS), and a heart rate that matches the specific subtype (escape, accelerated, or tachycardia).
When should someone with junctional rhythm symptoms seek emergency care?
Seek immediate help if you experience fainting, severe chest pain or shortness of breath, or a heart rate below 40 bpm accompanied by dizziness or confusion.
What treatment options exist for symptomatic junctional rhythm?
Treatment starts with identifying reversible causes (medication adjustments, electrolyte correction). If symptoms persist, options include atropine or isoproterenol for acute management, and permanent pacemaker implantation for chronic symptomatic cases.