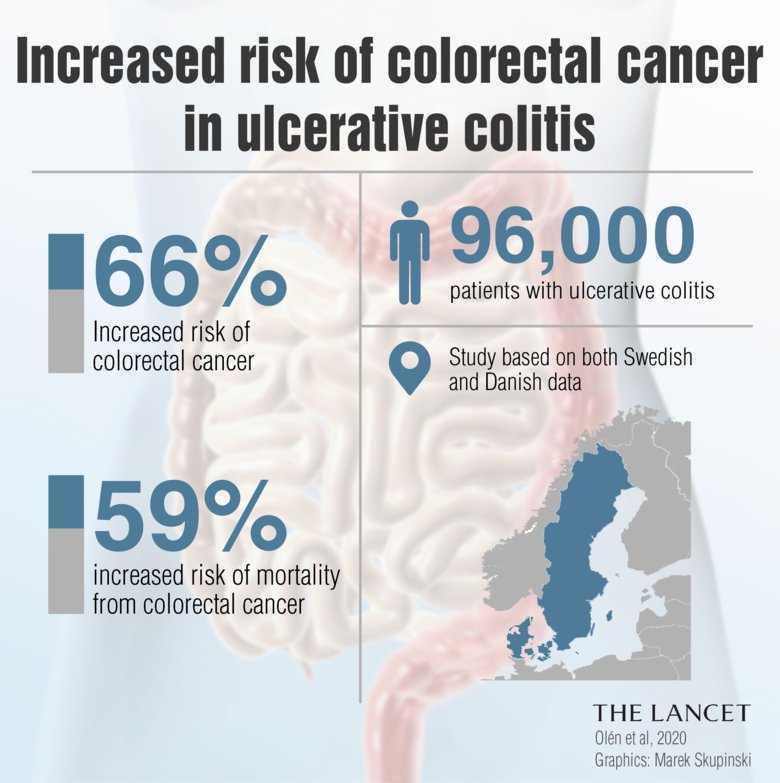
Hey there, friend. If youve been living with ulcerative colitis (UC) youve probably wondered, Whats the real chance that this condition could turn into cancer? The short answer is: the risk does rise over time, especially if the inflammation is extensive, but its not a guaranteed fate. Knowing the numbers, the warning signs, and the steps you can take helps you stay in control and keep anxiety at bay.
Understanding Baseline Risk
Lets start with the basics. Researchers have long measured how frequently people with UC develop colorectal cancer. A classic series reported roughly 2% after 10 years, 8% after 20 years, and 18% after 30 years of disease. More recent data, reflecting modern therapies and earlier detection, suggest a slightly lower riskabout 0.9% at 10 years and 3.5% at 20 years (according to a study).
Why the variation? It boils down to three big factors: how long youve had UC, how much of your colon is inflamed, and whether you have other conditions like primary sclerosing cholangitis (PSC). Below is a quick snapshot of overall percentages you might see quoted in different sources.
| Time Since Diagnosis | Risk of Colorectal Cancer |
|---|---|
| 010 years | 2% |
| 1020 years | 8% |
| 2030 years | 18% |
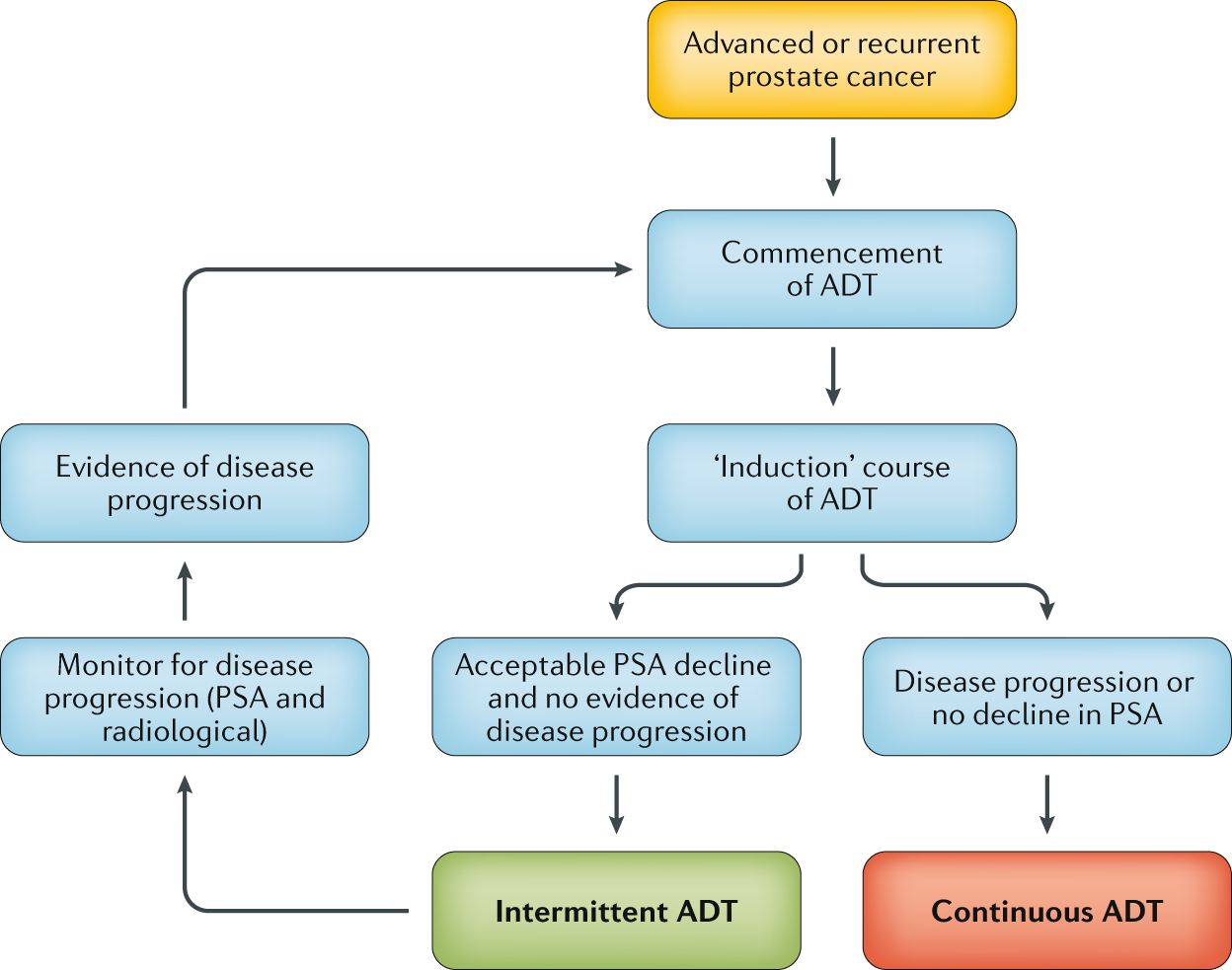
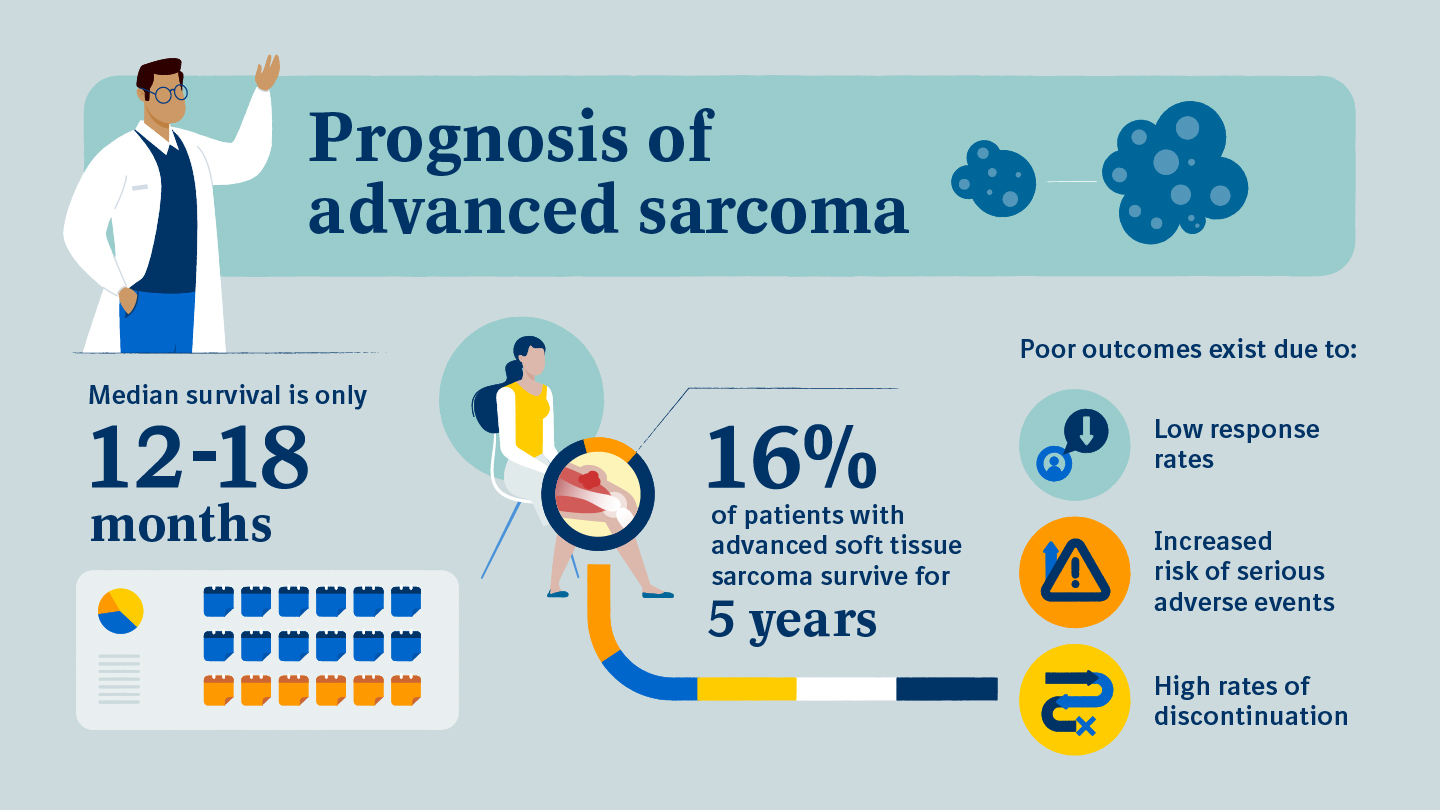
In simple terms: the longer you live with UC, the higher the oddsbut its still a minority of patients who actually develop cancer. Because questions on cancer span many specialties, those worried about outcomes in other cancerslike genitourinary casesmay find discussions on prostate removal life expectancy helpful when thinking about risks and survival factors in the context of cancer more broadly.
How does disease extent change risk?
Think of your colon like a road map. If the inflammation covers just the rectum, the road is short and the traffic (cancer risk) stays low. When UC spreads to the left side of the colonwhat doctors call leftsided ulcerative colitisthe risk jumps a bit, and with pancolitis (inflammation of the entire colon) it climbs even higher.
What percentage of UC patients actually get cancer?
Across large registries, between 1% and 2% of patients develop cancer within the first decade, rising to about 20% after three decades. Men tend to be a shade more vulnerable, and the presence of PSC can double the risk.
How does UC risk compare with Crohns disease?
Both are forms of inflammatory bowel disease, but the cancer numbers differ. UC carries roughly a 23fold increase in colorectal cancer risk, while Crohns disease (when it affects the colon) generally shows a 1.52fold increase (according to a review). So, if youve ever Googled Crohns vs ulcerative colitis cancer risk, thats the gist of it.
When UC Turns Cancer
How long does it take ulcerative colitis to turn into cancer?
Theres no exact calendar. Most cancers emerge after a decade or more of chronic inflammation. The latent period can be anywhere from 8 to 30 years, depending on how aggressively the disease is managed and personal risk factors.
Early cancer symptoms vs. UC flare symptoms
Unfortunately, UC flares and early colorectal cancer share some overlapblood in the stool, abdominal discomfort, and changes in bowel habits. The key is to watch for redflag twists that dont improve with your usual meds.
- Persistent rectal bleeding that lasts weeks despite treatment.
- Change in stool caliberthink pencilthin stools.
- Unexplained weight loss or night sweats, which are rarer in ordinary flares.
- New irondeficiency anemia discovered on routine blood work.
These are the ulcerative colitis cancer symptoms that should prompt a conversation with your gastroenterologist.
Quick symptom checklist
| Symptom | Likely UC Flare | Possible Cancer Warning |
|---|---|---|
| Blood in stool | (if persistent) | |
| Abdominal pain | ||
| Night sweats | ||
| Weight loss |
When in doubt, its always better to get checkedearly detection can mean a much simpler treatment path. If you have questions about cancer risk in the context of genetics, the field of colon cancer genetic testing is rapidly evolving and may inform your risk assessment or surveillance plan.
Factors Modifying Risk
Diseaserelated factors
Duration, extent (leftsided vs. pancolitis), severity, and the presence of PSC are the heavyweight champs in the risk arena.
Lifestyle & demographic modifiers
Sex mattersmen have a slightly higher incidence. Smoking is a weird one: it seems to protect against UC flareups but worsens overall cancer odds, so we dont recommend picking it up. Diet rich in fiber, regular exercise, and maintaining a healthy weight can all tilt the odds in your favor. For patients who have other conditions, such as kidney issues, considering nutrition is also vital and the advice from Renal cancer nutrition may offer additional insights for disease management.
Treatmentrelated influences
Good news: many medications do more than quiet inflammation; they also appear to lower cancer risk. Longterm 5ASA (mesalamine) therapy has been linked to a modest reduction in dysplasia, and biologics that keep inflammation in check are thought to indirectly protect the colon.
Risk comparison table
| Population | 10yr Risk | 20yr Risk | 30yr Risk |
|---|---|---|---|
| General (no IBD) | 0.2% | 0.5% | 0.8% |
| Ulcerative colitis | 2% | 8% | 18% |
| Crohns disease (coloninvolved) | 1% | 4% | 10% |
These numbers show why surveillance is a cornerstone of care for UC patients.
Surveillance & Detection
Who should get colonoscopic surveillance and when?
Guidelines from major societies (e.g., American Gastroenterological Association) suggest starting colonoscopy 810 years after diagnosis, sooner if you have PSC or extensive leftsided disease. After that, the interval depends on what the last exam foundusually every 13 years.
What does a surveillance colonoscopy involve?
Modern colonoscopies are highdefinition, and many doctors now use chromoendoscopya dye that highlights abnormal cells. Random biopsies are still taken, but targeted biopsies of any suspicious pits are the gold standard.
Stepbystep guide for patients
- Schedule the exam: Your gastroenterologist will set a frequency based on personal risk.
- Prep yourself: Follow the bowelcleanse instructions to the letter; a clear colon is the best canvas.
- During the procedure: The endoscopist will look for any discoloration, polyps, or flat lesions. If something looks off, theyll take a bitesized tissue sample.
- After the exam: Pathology results come back in a week or two. If dysplasia (precancer) is found, a treatment plan is discussed.
When is surgery recommended?
If highgrade dysplasia is detected, or if cancer is already present, a colectomy (removal of the colon) often becomes the safest option. Some earlystage cancers can be treated with chemoradiation, but surgery remains the most definitive cure for UCrelated cancer.
Emotional & Lifestyle Impact
Balancing benefits vs. risks
Its easy to feel torn between the inconvenience of frequent colonoscopies and the peace of mind they bring. Think of surveillance as a regular oil change for your colonsometimes annoying, always worthwhile for longterm health.
Realworld stories
Story 1: Maya, 38, was diagnosed with leftsided ulcerative colitis at 24. She stuck to a strict colonoscopic schedule and, at year 12, a tiny area of highgrade dysplasia was spotted. She opted for a preventive colectomy, and today shes thriving, cancerfree, and grateful she listened to her doctor.
Story 2: Tom, 52, delayed his first surveillance colonoscopy because work was busy. At year 15, he presented with a change in stool caliber and weight loss. A colonoscopy revealed stageII cancer. Though treatment was successful, Tom wishes hed acted sooner.
These anecdotes illustrate the power of early detection and the emotional relief that comes with knowing youre doing everything possible.
Resources & support groups
Living with UC isnt a solo journey. The Crohns & Colitis Foundation hosts online forums where folks share experiences about surveillance, diet, and coping strategies. Bowel Cancer Australia offers a helpline for those navigating a cancer diagnosis. Connecting with others can turn uncertainty into shared strength.
Remember, youre not alone, and the medical community is constantly refining ways to keep you safe.
Takeaway: Knowledge is your best ally. By understanding the numbers, watching for symptoms, and staying on top of surveillance, youll dramatically improve your odds of catching any trouble early.
Key Takeaways
Ulcerative colitis does raise your colorectalcancer riskabout 2% after ten years, climbing toward 20% after thirty. The odds depend on disease extent, duration, and additional factors like PSC. Watch for persistent bleeding, changes in stool shape, unexplained weight loss, or new anemia, and bring these to your doctors attention right away.
Regular colonoscopic surveillance (starting 810 years after diagnosis) is the most effective tool we have. Treatment advancesespecially 5ASA and biologicscan lower inflammation and, by extension, cancer risk. And while the journey can feel heavy, sharing experiences with friends, support groups, and trusted clinicians turns data into hope.
So, whats your next step? If you havent spoken to your gastroenterologist about a surveillance schedule, nows a perfect moment. Got questions about symptoms or lifestyle tweaks? Drop a comment below, or reach out to a local IBD support community. You deserve clear answers, compassionate care, and a future where ulcerative colitis is a part of your storynot the headline.
FAQs
What is the overall ulcerative colitis cancer risk over time?
Studies show roughly 2 % risk after 10 years, about 8 % after 20 years, and close to 18‑20 % after 30 years of disease. Modern data with better treatment suggest the risk may be slightly lower, around 0.9 % at 10 years and 3.5 % at 20 years.
How often should I undergo colonoscopic surveillance?
Guidelines recommend starting surveillance colonoscopy 8‑10 years after UC diagnosis. If the colon is extensively inflamed or you have primary sclerosing cholangitis, begin earlier. After the initial exam, repeat every 1‑3 years depending on findings.
Which symptoms might indicate cancer rather than a typical UC flare?
Red‑flag signs include persistent rectal bleeding despite treatment, pencil‑thin stools, unexplained weight loss, night sweats, and new iron‑deficiency anemia. Any of these should prompt immediate medical evaluation.
Can medication lower my ulcerative colitis cancer risk?
Yes. Long‑term 5‑ASA (mesalamine) use has been linked to a modest reduction in dysplasia, and biologic therapies that keep inflammation under control indirectly reduce cancer risk.
Does having primary sclerosing cholangitis (PSC) affect my cancer risk?
PSC roughly doubles the risk of colorectal cancer in UC patients. Those with PSC should start colonoscopic surveillance earlier (often at diagnosis) and may need exams every year.