Im not a doctor, but Ive spoken with oncologists, reviewed the latest guidelines, and heard stories from people living with stage4 mouth cancer. Below is a clear, nofluff guide that gives you the facts you need right now.
What Is Stage 4?
How does the TNM system define stage4 oral cancer?
The TNM classification looks at three things: the size of the primary tumor (T), whether the cancer has reached nearby lymph nodes (N), and whether it has spread to distant organs (M). In stage4, one or more of the following is true:
| Component | Definition | What it Means for You |
|---|---|---|
| T4a | Tumor invades nearby structures (e.g., bone, deep muscles) | More complex surgery may be needed |
| T4b | Tumor invades critical areas (e.g., base of skull, pterygoid plates) | Often requires combined modality treatment |
| N2N3 | Multiple or large lymphnode groups involved | Higher risk of distant spread |
| M1 | Distant metastasis (lung, liver, bone) | StageIVc systemic therapy becomes central |
Is stage4 mouth cancer curable?
Curable is a nuanced word. While a true cure is rare at this stage, many patients achieve longterm remission with aggressive, multidisciplinary treatment. The goal often shifts to controlling the disease, preserving function, and maintaining quality of life.
Recognizing Symptoms Now
What are the most common stage4 oral cancer symptoms?
Because the disease is advanced, symptoms tend to be more pronounced than in early stages. Look out for:
- Persistent ulcer or sore that wont heal for more than three weeks
- Unexplained swelling of the jaw, neck, or tongue
- Difficulty swallowing or a feeling that something is stuck
- Numbness or tingling in the mouth, lip, or facial area
- Bleeding, loose teeth, or a frozen feeling in the jaw
- Unexplained weight loss and fatigue
How do these differ from stage1 oral cancer symptoms?
Earlystage disease (stage1) often shows only a small, painless lesion or a mild change in texture. In contrast, stage4 symptoms are usually painful, cause functional problems, and may be accompanied by visible swelling or nerve involvement.
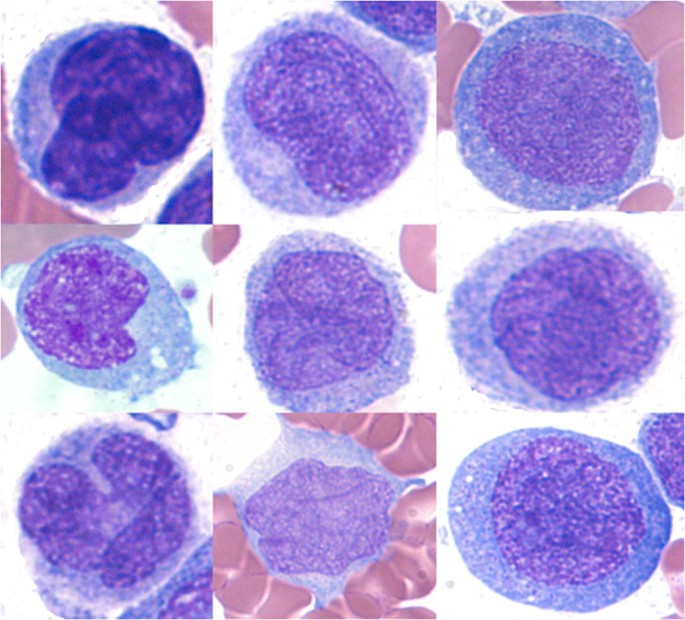
First signs of mouth cancer pictures
Seeing visual references can help you spot early warning signs. Trusted health sites such as the provide clear oral cancer stages pictures that illustrate how a lesion progresses from a small white patch to a larger ulcerated area.
Life Expectancy Stats
What is the average stage4 oral cancer life expectancy?
Statistical averages are just thataverages. According to data from the National Cancer Institute, the median overall survival for stage4 headandneck cancers hovers around 1824 months when treated with modern multimodal therapy. However, many factors shift this number:
- Patient age and overall health
- HPV status (HPVpositive tumors often respond better)
- Extent of metastasis (local vs. distant)
- Choice and timing of treatment
How does this compare with stage3 oral cancer survival rate?
Stage3 disease usually shows a 5year survival rate of about 5060%, while stage4 drops to roughly 3040% according to a review. The gap highlights why early detection is so critical.
Treatment Options Overview
What are the main stage4 mouth cancer treatment modalities?
Because the cancer has spread, a single approach rarely suffices. The most common combination includes:
- Surgery removal of the primary tumor and affected lymph nodes when feasible.
- Radiation therapy often delivered as intensitymodulated radiation therapy (IMRT) to spare healthy tissue.
- Chemotherapy drugs like cisplatin or carboplatin given concurrently with radiation (chemoradiation).
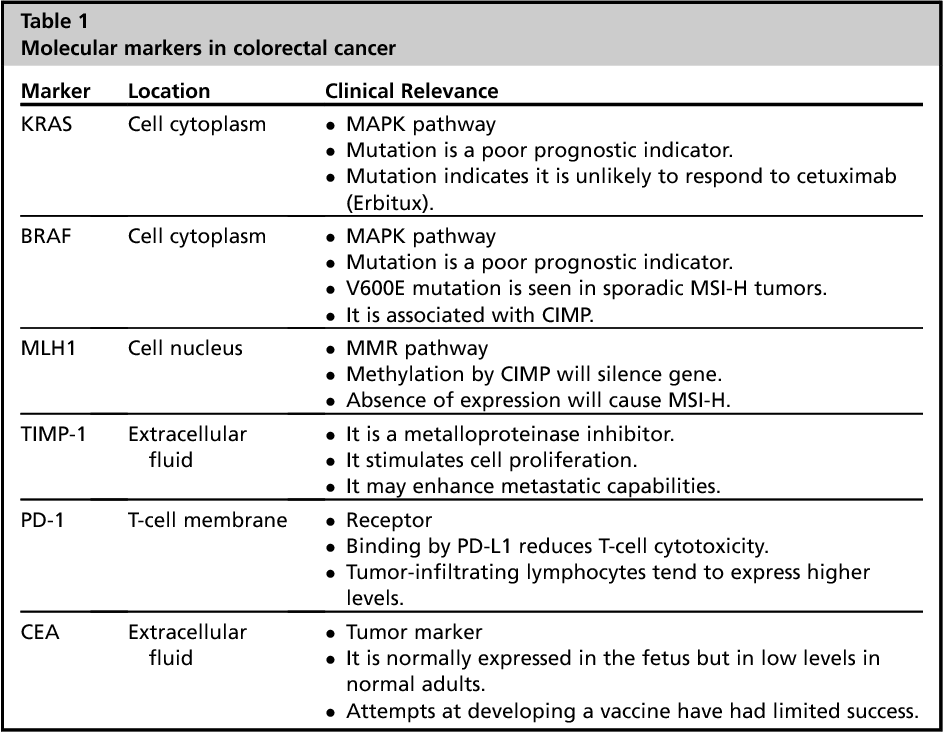
- Targeted therapy agents such as cetuximab that hone in on specific cellular pathways.
- Immunotherapy PD1 inhibitors (pembrolizumab, nivolumab) that boost the bodys own immune response.
Is surgery still an option at stage4?
When the tumor is resectable (e.g., T4a without extensive skull involvement), surgery can dramatically reduce tumor burden and improve the effectiveness of subsequent radiation or systemic therapy. In unresectable cases, doctors lean on chemoradiation and immunotherapy.
What does stage4 mouth cancer treatment look like in practice?
Imagine a threeact play:
- Act1 Neoadjuvant therapy: Chemotherapy or immunotherapy given first to shrink the tumor.
- Act2 Surgery (if possible): The surgeon removes the remaining disease, often followed by reconstruction using tissue from the forearm or thigh.
- Act3 Adjuvant therapy: Radiation (sometimes with additional chemo) to eradicate microscopic cells.
Comparison of Treatment Efficacy & SideEffects
| Modality | Typical Success Rate (local control) | Common SideEffects | Typical Duration |
|---|---|---|---|
| Surgery | 6080% (if resectable) | Swallowing difficulty, speech changes, scar tissue | 48weeks (postop recovery) |
| Radiation (IMRT) | 5070% | Mucositis, dry mouth, skin irritation | 67weeks |
| Chemotherapy (cisplatin) | Enhances radiation by 1015% | Nausea, kidney strain, hearing loss | Concurrent with radiation |
| Immunotherapy | 1020% durable responses in advanced cases | Fatigue, skin rash, endocrine disorders | Every 23weeks, ongoing |
Can emerging therapies improve outlook?
Yes. Clinical trials are testing combinations of immunotherapy with radiation to boost the immune systems ability to recognize tumor cells. Some patients in earlyphase studies have experienced surprisingly long remission periods, offering a glimmer of hope for future standards of care.
Weighing Benefits & Risks
What are the biggest benefits of aggressive treatment?
When treatment succeeds, patients may:
- Regain the ability to speak and swallow more comfortably
- Achieve diseasefree intervals lasting several years
- Reduce the chance of further metastasis
What risks should you discuss with your care team?
Every powerful weapon brings collateral damage:
- Swallowing difficulties that may require a feeding tube
- Permanent changes in taste and dry mouth (xerostomia)
- Potential longterm facial disfigurement after surgery
- Radiationinduced secondary cancers (rare but real)
Checklist: Questions to Ask Your Doctor
- What is the exact TNM stage of my tumor?
- Which treatment combination do you recommend and why?
- What are the shortterm and longterm sideeffects I should expect?
- Are there any clinical trials that fit my profile?
- How will treatment affect my daily lifework, eating, speaking?
Living With The Diagnosis
Where can patients find reliable support?
Beyond the medical team, several organizations offer counseling, nutrition advice, and peertopeer forums. The , , and local headandneck cancer support groups can be lifelines.
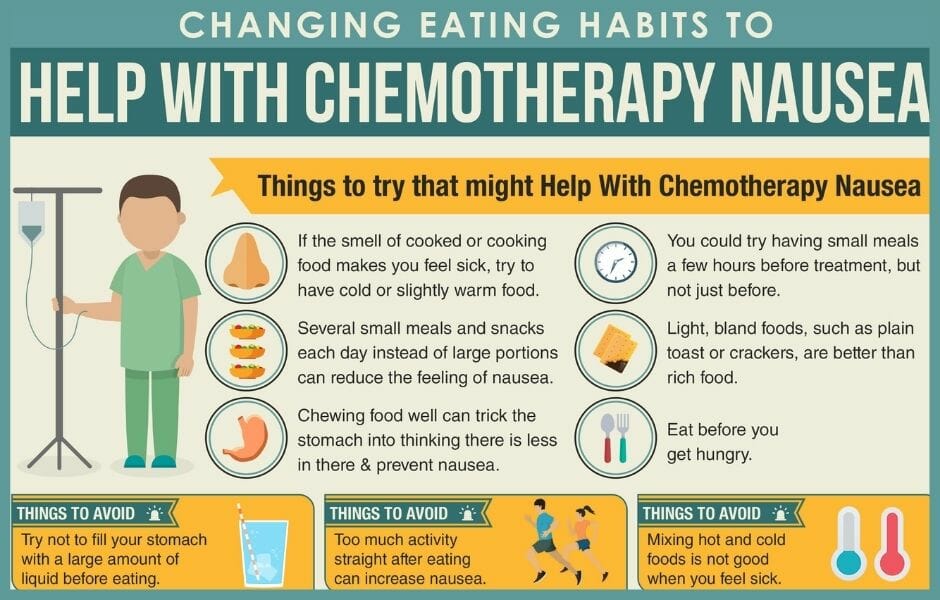
What lifestyle tweaks help during treatment?
- Nutrition: Soft, highprotein foods (smoothies, Greek yogurt, scrambled eggs) keep calories up without irritating sores.
- Oral hygiene: Gentle brushing with a soft brush, fluoride rinse, and avoiding alcoholbased mouthwashes.
- Physical activity: Light walking or stretching can reduce fatigue and maintain muscle tone.
- Mental health: Mindfulness, journaling, or therapy helps process the emotional rollercoaster.
Realworld example
Mark, a 58yearold former teacher, was diagnosed at stage4 after a persistent ulcer turned out to be cancerous. He chose a combined approach: two cycles of neoadjuvant immunotherapy, followed by surgery and postop radiation. Today, three years later, he enjoys weekly guitar lessons and runs a small book club for other survivors. His story illustrates how a wellplanned, multidisciplinary regimen can buy meaningful time and quality of life.
Stage4 mouth cancer is undeniably serious, but it is not a hopeless sentence. By understanding exactly what stage4 entails, recognizing the hallmark symptoms, and weighing the realistic lifeexpectancy figures, you can make empowered decisions. Modern treatmentsurgery, radiation, chemotherapy, targeted agents, and immunotherapyoffers a toolbox that, when applied thoughtfully, can shrink tumors, extend survival, and preserve dignity.
Remember, you are not alone. Connect with reputable cancer centers, ask the hard questions, lean on support groups, and take small, daily steps toward nutrition and wellbeing. If you have questions or want to share your own journey, feel free to comment below. Lets walk this road together.
For readers also facing cancer treatment decisions elsewhere in the body, resources about Cancer diet plan can help manage nutrition during therapy.
FAQs
What are the most common signs that mouth cancer has advanced to stage 4?
Typical stage 4 symptoms include a persistent ulcer that won’t heal, noticeable swelling of the jaw or neck, difficulty swallowing, numbness or tingling in the face, frequent bleeding, loose teeth, significant weight loss, and constant fatigue.
How does the TNM system define stage 4 oral cancer?
Stage 4 is assigned when any of the following occur: T4a (tumor invades bone or deep muscles), T4b (tumor reaches critical structures like the base of the skull), N2‑N3 (large or multiple lymph‑node groups involved), or M1 (distant metastasis to organs such as lung, liver, or bone).
Which combination of treatments provides the best chance of disease control for stage 4 mouth cancer?
Most experts recommend a multimodal approach: neoadjuvant chemotherapy or immunotherapy to shrink the tumor, followed by surgery (if resectable) and then adjuvant radiation—often with concurrent cisplatin or a targeted agent. Adding PD‑1 inhibitors (pembrolizumab or nivolumab) can improve outcomes in many patients.
Is stage 4 mouth cancer curable, or is the goal only to manage it?
Complete cure is uncommon at this stage, but aggressive, coordinated therapy can lead to long‑term remission for a substantial number of patients. The primary goals become controlling the disease, preserving speech and swallowing function, and maintaining quality of life.
Where can patients find reliable support and resources during treatment?
Key resources include the American Cancer Society, Mayo Clinic’s oral‑cavity cancer program, the Oral Cancer Foundation, and local head‑and‑neck support groups. They offer counseling, nutrition advice, peer‑to‑peer forums, and information about clinical trials.