ADHD starts in the brain. Differences in the prefrontal cortex, basal ganglia, and anterior cingulate, plus imbalances of dopamine and norepinephrine, are the main drivers of the symptoms you see.
Knowing the brain-based causes helps you spot the signs early, choose the right treatment, and avoid myths that can waste time and money.
Core Neurobiology
Which brain regions are underdeveloped or miswired?
The brain isn't broken; it's just wired a little differently. In most people with ADHD, the prefrontal cortexthe part that handles planning, impulse control, and focustends to be smaller or slower to mature. The basal ganglia, which regulate movement and reward, also show reduced activity, and the anterior cingulate cortex (the emotional-attention hub) often lights up less during demanding tasks.
Key Brain Areas
Below is a quick snapshot of the main regions that tend to differ in an ADHD brain.
| Region | Typical Role | ADHD Difference |
|---|---|---|
| Prefrontal Cortex | Executive functions, decision-making | Reduced thickness, delayed maturation |
| Basal Ganglia | Movement, reward processing | Lower activation, altered connectivity |
| Anterior Cingulate Cortex | Attention, emotional regulation | Less consistent firing during tasks |
Which neurotransmitters are out of balance?
Dopamine and norepinephrine are the messenger chemicals that keep our brain's attention circuitry humming. In ADHD, dopamine transmission is often too low, which makes it harder to stay on task or feel motivated. Norepinephrine, which helps sharpen focus, can also be underactive.
Why those chemicals matter
Think of dopamine as the reward fuel that tells your brain, "hey, this is worth doing." When the tank runs low, staying motivated feels like pushing a boulder uphill. Norepinephrine is the alert switchwhen it's dim, even simple chores can feel foggy.
How do these changes translate into everyday symptoms?
When the prefrontal cortex is sluggish and dopamine's running low, you might find yourself drifting off in class, forgetting appointments, or impulsively buying that gadget you don't need. The basal ganglia's move-on-autopilot can cause fidgeting or the restless urge to get up during meetings. Notably, conditions like restless legs ADHD highlight how overlap between neurological pathways can manifest as both motor restlessness and attentional challenges in some individuals.
ADHD Brain vs. Regular Brain
| Feature | Regular Brain | ADHD Brain |
|---|---|---|
| Prefrontal Cortex Size | Fully matured by early adulthood | Smaller, matures later |
| Dopamine Activity | Balanced, steady | Reduced, erratic |
| Baseline Alertness | Consistent | Fluctuating, easily distracted |
Genetics Blueprint
What genes are linked to ADHD?
Science has pinpointed a handful of risk genes. The most talked-about are DRD4 (a dopamine receptor), DAT1 (a dopamine transporter), and SNAP25 (involved in neurotransmitter release). These genes don't guarantee ADHD, but they tilt the odds.
Genetic Snapshot
- DRD4 7-repeat allele: linked to higher novelty-seeking.
- DAT1 10-repeat: may reduce dopamine reuptake efficiency.
- SNAP25: affects how well signals travel between neurons.
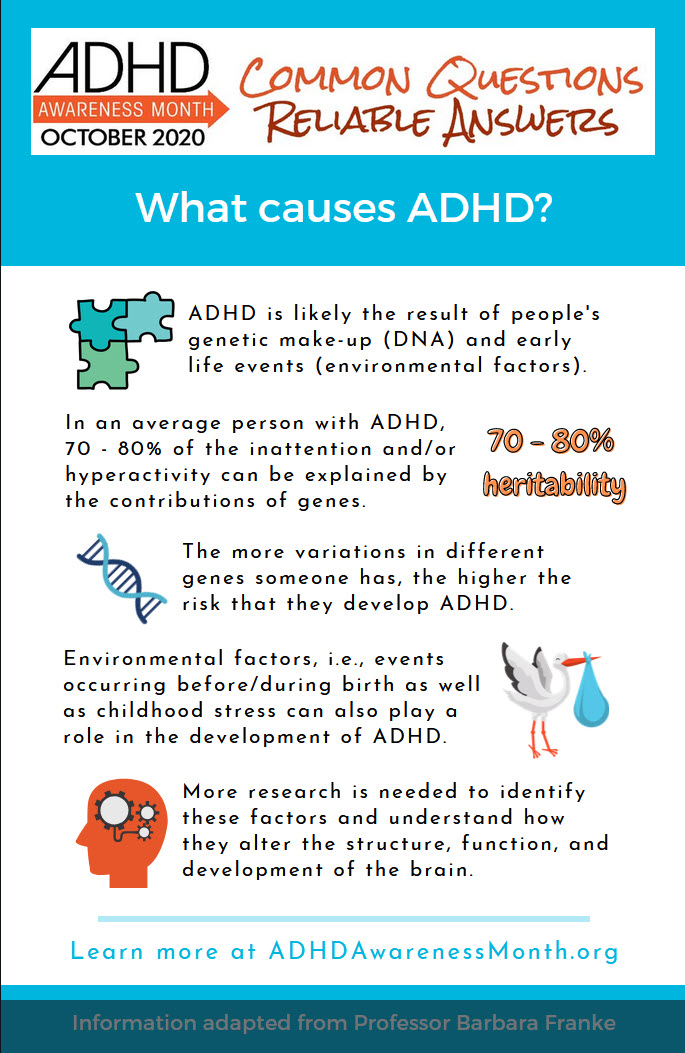
How hereditary is ADHD?
Twin studies consistently show about 70% heritability. That means if one identical twin has ADHD, the other has a roughly seven-in-ten chance of sharing the diagnosis. Family histories often reveal the patternparents, siblings, even grandparents may have had attention challenges.
Family-History Checklist
Ask yourself:
- Did a parent or grandparent struggle with focus?
- Do you notice similar quirks in siblings?
- Has anyone in the family responded well to stimulant medication?
Can genetics explain adult-onset ADHD?
Adult-onset cases often hide a latent genetic risk that surfaces when life throws new stressorscollege, a demanding job, or a major life change. The underlying brain wiring may have been there all along, but the environment finally nudges it into the spotlight.
Environmental Triggers
What prenatal and early-life factors raise risk?
It's not just your DNA; the environment matters too. Low birth weight, premature birth, and exposure to nicotine or alcohol while in the womb can all increase ADHD odds. Even lead exposure in early childhood has been linked to attention difficulties.
Quick Prevention Tips
- Avoid smoking or drinking during pregnancy.
- Ensure a safe, lead-free home environment.
- Promote regular pediatric checkups for early detection.
How do sleep, diet, and stress play a role?
Sleep deprivation can mimic ADHD symptomsthink foggy brain, irritability, and wandering thoughts. Poor nutrition, especially low omega-3 fatty acids, may worsen dopamine function. Chronic stress can amplify the brain's fight-or-flight mode, making it harder for the prefrontal cortex to stay in control.
My personal anecdote
I once tried to power through a week of all-night study sessions, only to realize my focus was crumbling faster than a cookie in milk. A quick nap and a salmon dinner (rich in omega-3) revived my mental sharpnessproof that lifestyle tweaks truly matter.
Psychological causes vs. brain causes
When people say psychological causes, they often mean trauma, anxiety, or depression that coexists with ADHD. These factors don't replace the neurobiology; they interact with it. A child who's constantly stressed may see their already-fragile dopamine system further taxed.
Case study snapshot
Emily, a 10-year-old, struggled with homework and was labeled lazy. A neuropsychologist discovered that a recent move and school bullying had heightened her cortisol (stress hormone) levels, which in turn dulled her dopamine pathways. With counseling and a low-dose stimulant, her grades jumped.
Kids vs. Adults
What does the ADHD brain look like in kids?
In children, imaging shows reduced cortical thickness in the prefrontal area and heightened activity in the default-mode network (the brain's idle mode). This makes it harder for kids to stay on task, leading to classic hyperactivity and impulsivity. It's also worth noting that ADHD presents differently in children compared to adults, with core ADHD biology findings underpinning these differences.
Kids vs. Adults Core Findings
| Aspect | Children | Adults |
|---|---|---|
| Prefrontal Maturity | Delayed | Often still underactive |
| Default-Mode Network | Overactive during tasks | Continues to intrude on focus |
| Symptoms | Hyperactivity, impulsivity | Inattention, restlessness |
How does the adult ADHD brain differ?
Adults tend to show reduced connectivity in reward circuits and a less efficient cognitive control network. The hyperactive motor component often mellows, but the mental restlessness can feel like an endless mental hum.
Why symptoms change with age
As the brain ages, the prefrontal cortex finally catches upjust a bitso overt hyperactivity fades. However, the dopamine deficiency may remain, so adults still wrestle with procrastination, time-blindness, and rumination.
From Cause to Treatment
How do stimulant meds fix neurotransmitter gaps?
Stimulants like methylphenidate (Ritalin) and amphetamines (Adderall) block dopamine reuptake, flooding the synapse with more focus fuel. This short-term boost lets the prefrontal cortex function more like a well-tuned engine.
Medication Snapshot
- Onset: 3060 minutes for most oral forms.
- Effect size: Improves core symptoms by ~3040% vs. placebo (study).
- Common side effects: Appetite loss, insomnia, mild increase in heart rate.
Nonpharmacologic options that reshape brain wiring
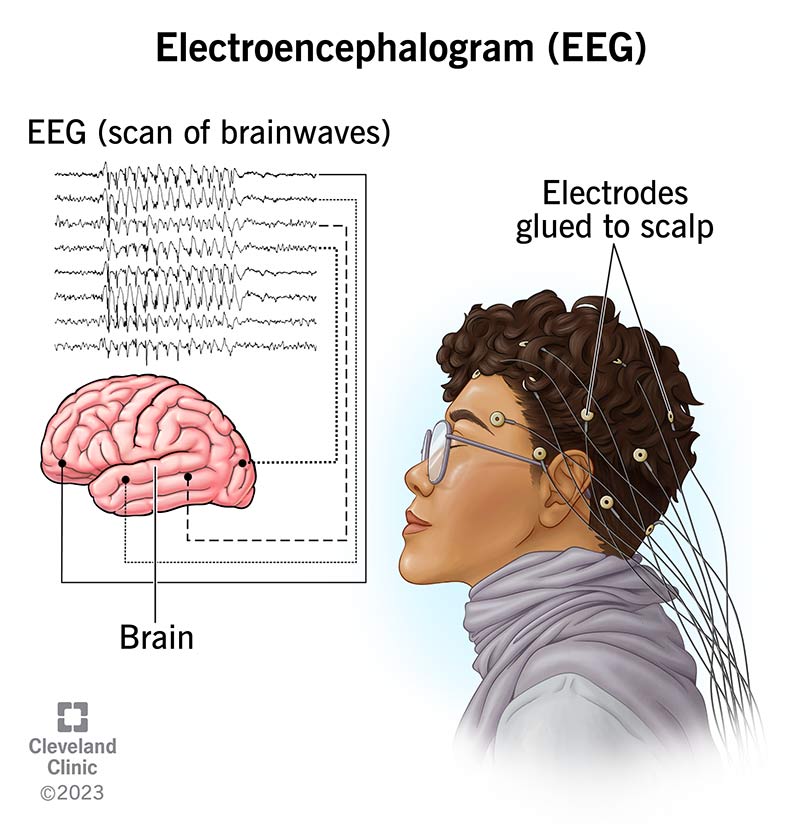
Medication isn't the whole story. Cognitive-behavioral therapy (CBT) trains the prefrontal cortex to plan, prioritize, and self-monitoressentially giving the brain a workout. Exercise, especially aerobic activity, boosts dopamine production, while neurofeedback teaches you to control brainwave patterns in real time. For an overview of the core biology involved in ADHD and related treatment approaches, see ADHD biology.
Evidence-based alternatives
- CBT: Meta-analyses show a 20% additional symptom reduction when combined with meds.
- Exercise: 30 minutes of moderate cardio can raise dopamine by up to 30%.
- Neurofeedback: RCTs report improved attention scores after 2030 sessions.
Can ADHD be cured?
Calling it a cure can be misleading. ADHD is a lifelong neurodevelopmental condition, but the brain is plastic. With proper treatment, many people achieve functional remissionmeaning symptoms no longer interfere significantly with daily life. It's more about management and adaptation than a permanent wipeout.
Real-world story
Mark, 34, was diagnosed at 27 after struggling at work. After a year of low-dose stimulant, weekly CBT, and nightly runs, he describes his life as "back on track." He still uses a planner, but the frantic feeling is gone.
Common Myths
Is ADHD just bad parenting or lack of willpower?
Absolutely not. Brain imaging and genetic studies show that ADHD is rooted in biology, not parenting style. Good parenting can support coping strategies, but it doesn't fix the underlying dopamine deficit.
Do diet-only cures work?
Elimination diets may help a small subset of children with food sensitivities, but they're not a universal remedy. A balanced diet rich in omega-3s, protein, and complex carbs supports neurotransmitter health, yet it's only one piece of the puzzle.
Is ADHD a modern disease?
Historical records describe restless or inattentive children centuries ago. The label has evolved, but the brain differences have been there all along.
Practical Takeaways
Self-Screen Checklist
Ask yourself:
- Do I often lose track of time?
- Is starting tasks a constant battle?
- Do I feel a surge of restlessness when sitting still?
- Has anyone ever described me as impulsive or scatterbrained?
If you answered yes to several, a professional evaluation could be worthwhile.
When to Seek Professional Help
Look for red-flag patterns:
- Persistent academic or work underperformance despite effort.
- Relationship strains linked to forgetfulness or impulsivity.
- Co-occurring anxiety, depression, or substance use.
Consider consulting a child psychiatrist, adult psychiatrist, or a licensed neuropsychologist.
Resources & Further Reading
- American Academy of Child and Adolescent Psychiatry
- National Institute of Mental Health ADHD Overview NIH
- CHADD Education and Support for ADHD
Conclusion
The brain is at the heart of ADHDgenetics set the stage, while environment and life experiences fine-tune the wiring. Knowing what causes ADHD in the brain empowers you to spot the signs early, choose evidence-based treatments, and ditch the myths that keep us stuck. Got more questions? Share your story in the comments, or reach out if you need a friendly nudge toward the right help. We're all in this together.
FAQs
What brain regions are most affected by ADHD?
The pre‑frontal cortex, basal ganglia, and anterior cingulate cortex typically show reduced size or activity, leading to challenges with attention, impulse control, and emotional regulation.
How do dopamine and norepinephrine contribute to ADHD symptoms?
Dopamine drives motivation and reward; low levels make tasks feel unrewarding. Norepinephrine sharpens alertness; when it’s under‑active, focus drifts and mental fog appears.
Is ADHD mainly inherited or caused by the environment?
Both play roles. About 70 % of the risk is genetic, but prenatal exposures (e.g., nicotine, low birth weight) and early‑life factors (lead, stress, poor sleep) can amplify or trigger symptoms.
Can lifestyle changes improve the brain chemistry of someone with ADHD?
Yes. Regular aerobic exercise, adequate sleep, and a diet rich in omega‑3 fatty acids can boost dopamine production and help the pre‑frontal cortex work more efficiently.
Are stimulant medications a permanent fix for ADHD?
Stimulants temporarily correct neurotransmitter imbalances, providing noticeable symptom relief. Long‑term management usually combines medication with therapy, exercise, and environmental adjustments; they do not “cure” the underlying neurodevelopmental differences.