Hey there If you're a nurse who just learned a patient has gestational diabetes (GDM), you might be wondering how to jump from what now? to a solid, supportive care plan fast. In the next few minutes, we'll walk through exactly what you need: the key assessments, the right NANDA diagnoses, practical interventions, and even free PDFs and PowerPoints you can share right away. Think of this as a friendly chat over coffee, not a textbook you have to slog through.
Understanding GDM Basics
What is gestational diabetes and why does it matter?
Gestational diabetes is high blood sugar that shows up during pregnancy, usually around weeks 24-28. It affects roughly 7-10% of pregnant people in the U.S., and if left unmanaged, it can lead to complications for both mom and babylike preeclampsia, cesarean delivery, macrosomia (big babies), and neonatal hypoglycemia. For example, understanding preeclampsia vs gestational hypertension can help in identifying and managing related risks. The good news? With the right nursing care, most women achieve healthy glucose levels and go on to have thriving newborns.
When you grasp the why behind the numbers, you'll feel more confident guiding patients through diet, meds, and monitoring. It also helps you explain the stakes in plain languagesomething every patient appreciates. Moreover, understanding stress gestational diabetes connections can aid in developing a comprehensive care plan.
Who's at higher risk?
Risk factors include a previous GDM pregnancy, a family history of type 2 diabetes, obesity (BMI 30), and certain ethnic backgrounds (e.g., Hispanic, South Asian, African American). Knowing these clues early lets you prioritize education and tighter glucose checks, similar to how you might manage risk factors for preterm birth, ensuring proactive measures are taken.
NANDA Diagnoses Overview
Which NANDA diagnoses fit gestational diabetes?
Here are the most common nursing diagnoses you'll encounter, paired with the defining characteristics you'll see on the floor.
| NANDA Diagnosis | Defining Characteristics | Desired Outcomes |
|---|---|---|
| Risk for unstable blood glucose | + Polyuria, random glucose >200mg/dL, frequent thirst | Maintain fasting glucose 95mg/dL and 2hr postprandial 140mg/dL |
| Imbalanced nutrition: more than body requirements | + Excessive carb intake, weight gain >15kg, cravings | Achieve appropriate pregnancy-specific weight gain (11-16kg) |
| Deficient knowledge (gestational diabetes) | + I don't know how to count carbs, lack of diet log | Demonstrate accurate carb counting and self-monitoring |
| Risk for ineffective breastfeeding | + Low milk supply concerns, anxiety about glucose control | Initiate breastfeeding within 1 hour of birth, maintain glucose <120mg/dL |
Leaning on the latest (2024) will give you up-to-date criteria and coding tips for charting.
How do I write a concise diagnosis statement?
Use the format: Risk for unstable blood glucose related to pancreatic cell dysfunction as evidenced by fasting glucose 110mg/dL and polyuria. Keeping it short helps the whole care team stay on the same page.
Building a Care Plan
What should a gestational diabetes nursing care plan include?
Think of a care plan as a roadmap: assessment diagnosis interventions evaluation. Below is a quick-click checklist you can copy into a Word document, PDF, or even a Scribd upload for your unit.
- Assessment: vitals, fasting & 2hr postprandial glucose logs, dietary recall, fetal growth scans, urine ketones.
- Diagnosis: select one or more of the NANDA codes above.
- Interventions:
- Blood-glucose monitoring: fasting, premeal, 2hr postmeal (4-6 checks/day).
- Nutrition teaching: carb counting, glycemic index, portion control.
- Physical activity: 30min moderate-intensity walking most days.
- Medication: insulin sliding scale or oral agents as per OBGYN order.
- Psychosocial support: address anxiety, provide counseling referrals.
- Evaluation: compare glucose values to target, review weight gain trajectory, check patient confidence with self-monitoring, document delivery outcomes.
When you hand a patient a tidy, printable PDF, they're more likely to stay engaged. You can even add a QR code linking to a quick-reference on GDM pathophysiology.
How do I personalize the plan for cultural differences?
Ask open-ended questions like, "What foods are staples in your household?" Then modify the carb-counting sheet to include familiar itemsthink roti, plantains, or corn tortillas. This cultural humility shows respect and improves adherence.
Core Nursing Interventions
How should I monitor glucose safely in the hospital and at home?
Inpatient: use a calibrated glucometer after the first meal, then every 4-6 hours. Record the 2-hour postprandial readingthis is the gold standard for GDM control. Outpatient: teach patients how to use a fingerstick device or continuous glucose monitor (CGM). Emphasize handwashing, site rotation, and proper disposal of lancets.
When is insulin therapy needed versus diet-only control?
If a patient's fasting glucose stays <95mg/dL and 2hr postprandial <140mg/dL after two weeks of diet/exercise, you can often continue with diet alone. But if numbers creep above those thresholds, or if there's a fasting glucose >126mg/dL, initiate insulin. The typical approach is a basal-bolus regimen, titrated according to a sliding-scale protocol you can embed in a deck for quick reference.
What education points lower postpartum complications?
1. Schedule a 6-week oral glucose tolerance test (OGTT) after delivery.
2. Encourage exclusive breastfeeding for at least 6 monthsit improves glucose regulation.
3. Discuss long-term lifestyle changes: balanced meals, regular activity, and weight management.
4. Provide a postpartum warning list (e.g., excessive thirst, frequent urination) so patients know when to call.
Mini PPT Outline You Can Export
| Slide | Key Content |
|---|---|
| 1 | GDM pathophysiology (simple graphic) |
| 2 | Monitoring schedulefinger stick vs. CGM |
| 3 | Insulin dosing algorithm (flowchart) |
| 4 | Nutrition counselingPlate Method handout |
| 5 | Postdelivery follow-up & breastfeeding tips |
Patient Education Tips
What are the top five things I should tell a pregnant client with GDM?
- Your blood sugar matters, but it's controllable. With proper diet, activity, and occasional medication, most women keep their levels in range.
- Carb counting is your new best friend. One slice of bread15g carbs; half a cup of rice22g carbs.
- Movement helps. A 30-minute walk after meals can lower postprandial spikes.
- Keep a log. Write down everything you eat, your glucose number, and how you feel.
- You're not alone. Ask for supportpartner, family, or a diabetes educator.
How can I make nutrition advice feel less diet and more lifestyle?
Swap cut carbs for choose smarter carbs. Show a visual guide: a fist-size portion of fruit, a cupped-hand portion of protein, and two-hand-wide servings of veggies. Offer recipe swapslike swapping white rice for quinoa or using Greek yogurt instead of sour cream.
Handout Ideas You Can Print
- Carb Counting Cheat Sheet (with pictures of common foods).
- Safe Exercise Log (track steps, mood, and glucose).
- Breastfeeding & GDM Tips (hydration, timing feeds after meals).
Monitoring Outcomes
Which outcome indicators prove my care plan is working?
Track these metrics during the pregnancy and at delivery. They also make excellent data for quality-improvement reports.
| Indicator | Target | Current Avg. | Action if Above Target |
|---|---|---|---|
| Fasting glucose 95mg/dL | 80% of readings | 78% | Review insulin sliding scale, increase diet counseling. |
| Maternal weight gain (kg) | 11-16kg total | 14kg | Reemphasize portion sizes, schedule dietitian consult. |
| Neonatal birth weight <4kg | 95% | 93% | Tighten glucose control in third trimester. |
According to a recent Gestational Diabetes Journal (2024), keeping fasting glucose under 95mg/dL reduces macrosomia risk by 30%.
How should I document adverse events?
Use the SOAP note format: Subjective (patient's symptoms), Objective (glucose numbers, vitals), Assessment (diagnosis), Plan (what you'll do next). Be clear, concise, and always include the time of eventthis helps the entire care team intervene quickly.
FAQs Quick Answers
Can I breastfeed if I have gestational diabetes?
Absolutely Breastfeeding actually helps stabilize maternal glucose. Just keep your own blood sugar in range and stay well-hydrated.
Do I need insulin if my diet looks perfect?
If after two weeks of strict diet and exercise your fasting glucose stays <95mg/dL and 2hr postprandial <140mg/dL, you may avoid insulin. Continuous monitoring is key, thoughnumbers can shift quickly.
How long after delivery will I need glucose testing?
Schedule a 6-week OGTT. If it's normal, repeat a fasting glucose or HbA1c at your 1-year postpartum visit. Most women revert to normal, but the risk of type 2 diabetes stays elevated.
What are the warning signs of neonatal hypoglycemia?
Look for jitteriness, poor feeding, lethargy, or a low body temperature. Quick glucose checks and early feeding usually fix the issue.
Free Resources & Tools
Where can I find ready-made GDM nursing care plan PDFs?
Here are a few trusted sources you can bookmark:
Which PowerPoint decks are free for maternity education?
Check out these decks that already include the slide outline from earlier:
All links point to reputable sites; feel free to download, customize, and share with your team.
Conclusion
Gestational diabetes can feel like a curveball, but with a clear nursing assessment, the right NANDA diagnoses, and a hands-on care plan, you become the steady guide your patients need. Use the printable PDFs, PPTs, and cheat sheets to keep information front-and-center, and always sprinkle in empathybecause behind every glucose reading is a person who deserves support. Got a story about a GDM patient who inspired you? Share it in the comments below, or let us know which resource helped you most. Together, we can make gestational diabetes nursing not just manageable, but truly empowering.
FAQs
What is a junctional rhythm and why does it occur?
A junctional rhythm is a heartbeat that originates from the AV node or His bundle instead of the SA node, usually because the SA node is suppressed or blocked.
Which medications are most likely to trigger a junctional rhythm?
Beta‑blockers, calcium‑channel blockers, digoxin (especially in toxicity), and anti‑arrhythmic drugs such as amiodarone or quinidine can slow the SA node and allow the AV node to take over.
How do electrolyte imbalances lead to a junctional rhythm?
High potassium levels depress SA‑node activity, while low potassium or magnesium can cause erratic pacing, both situations prompting the AV node to act as an escape pacemaker.
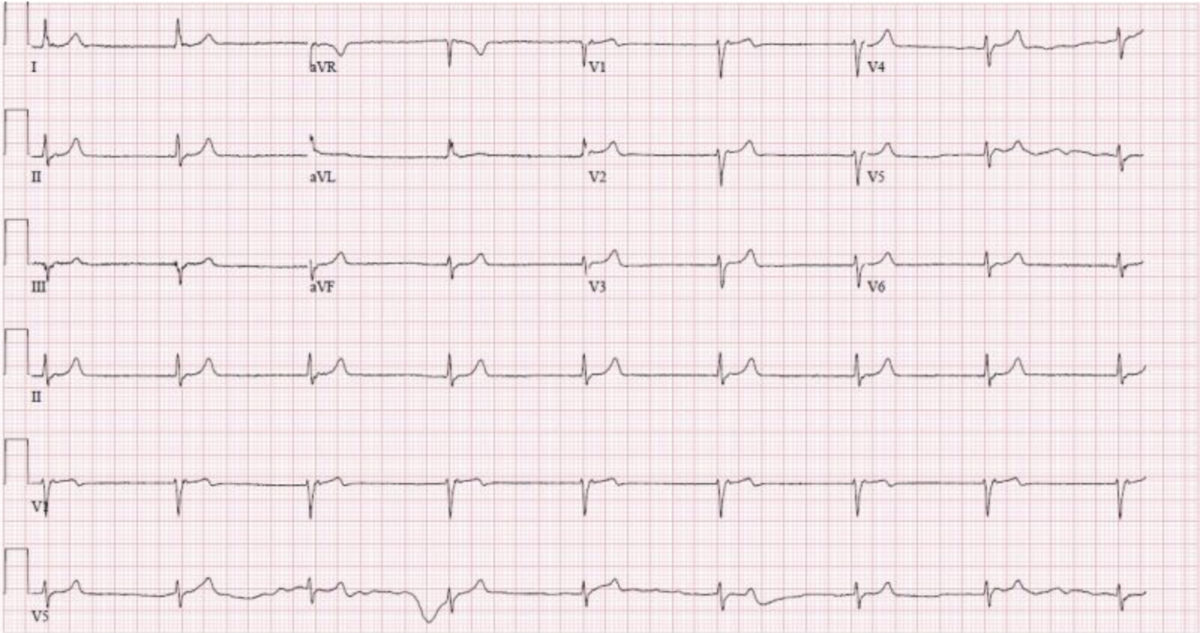
What does a junctional rhythm look like on an ECG?
Typical findings are a regular, narrow QRS complex with a rate of 40‑60 bpm (escape) or 60‑100 bpm (accelerated), and either absent P‑waves or retrograde P‑waves appearing after the QRS.
When is a permanent pacemaker recommended for junctional rhythm?
A pacemaker is considered if the underlying SA‑node dysfunction or high‑grade AV block persists, causing symptomatic bradycardia or recurrent junctional escape rhythms despite medical management.