Quick Overview Answer
Ever wondered why your heart sometimes takes a shortcut and beats from a different spot? Thats what we call a junctional rhythm. In plain language, its an arrhythmia where the electrical impulse that normally starts in the sinoatrial (SA) node skips over and originates from the atrioventricular (AV) node or the Hisbundle. Most of the time its harmless, showing up on an ECG as a steady beat without the usual P wave, and your body may not even notice. But occasionally it signals something deeper that needs a gentle nudge from a clinician.
Heres the skinny right away: a typical junctional rhythm runs between 4060 beats per minute (bpm) for an escape rhythm, and 60100bpm when its accelerated. If you catch it on a routine checkup, chances are youll be fine with just a watchful eye. If you feel lightheaded, dizzy, or notice an odd flutter, its time to get the ECG checked and dig a little deeper.
Why It Happens
What Triggers a Junctional Rhythm?
Think of the hearts electrical system as a relay race. The SA node normally hands the baton off first. When that runner tripsor when someone tampers with the batonthe AV node steps in. The usual suspects that cause this relay switch include:
- SAnode suppression from medication (betablockers, digoxin, calciumchannel blockers)
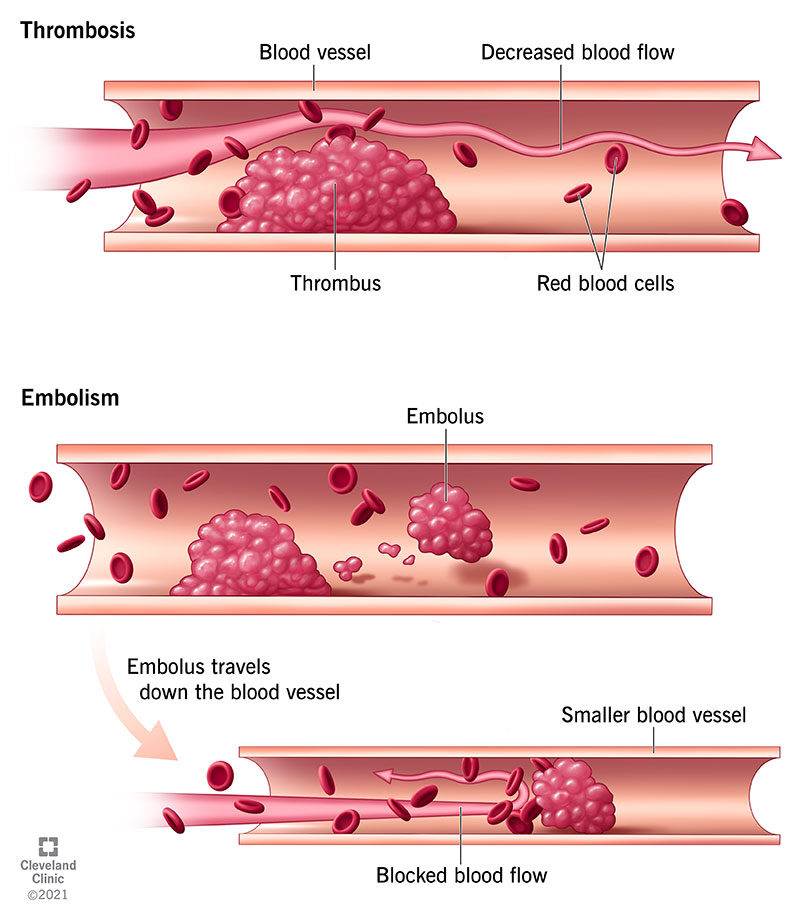
- Ischemic injury, especially after a heart attack that compromises the SA nodes blood supply
- Electrolyte imbalances, notably hyper or hypokalemia
- Thyroid disorders (both hypo and hyper)
- Postoperative changes after cardiac surgery
- Inflammatory conditions such as myocarditis or pericarditis
Less common triggers are things like severe hypoxia, Lyme disease, or even a sudden vagal surge when youre freaking out on a roller coaster. In each case, the AV nodes inherent automaticity rises enough to take over the pacing duty.
Common Causes at a Glance
| Cause | Typical Scenario | Frequency |
|---|---|---|
| Medication effect | Highdose digoxin or betablocker therapy | Moderate |
| Myocardial infarction | Anterior wall MI affecting SA node | High |
| Electrolyte disturbance | Hyperkalemia from renal failure | Lowmoderate |
| Thyroid dysfunction | Untreated hypothyroidism | Low |
| Postsurgical trauma | After bypass or valve replacement | High |
When youre writing a note for your doctor, mentioning any recent medication changes, surgeries, or lab results (especially potassium and thyroid labs) can help pinpoint the cause faster. If youve had recent cardiac procedures or are recovering from valve surgery, details about your heart valve recovery can be particularly relevant.
How Doctors Confirm the Diagnosis
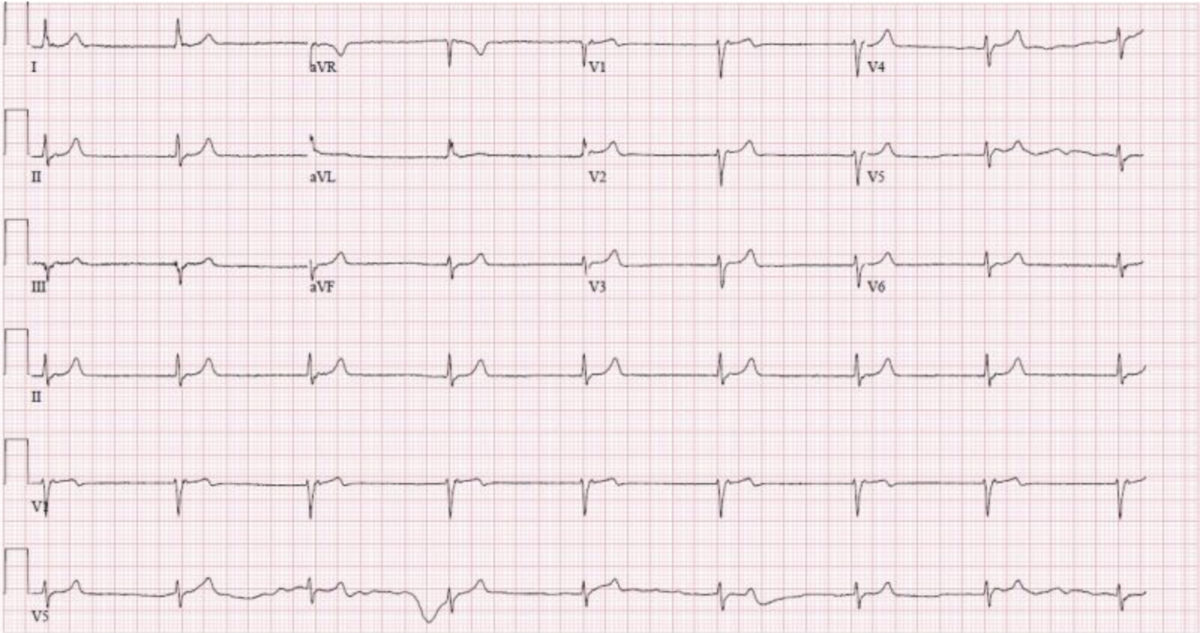
It all boils down to the . The classic hallmarks of a junctional rhythm are:
- Absent, inverted, or retrograde P waves (sometimes they hide behind the QRS complex)
- Regular, narrow QRS complexes (120ms)
- A rate that falls into one of two ranges: 4060bpm (escape) or 60100bpm (accelerated)
Thats why the phrase junctional rhythm ECG characteristics mattersrecognizing these subtle clues can spare you an extra round of tests.
How It Feels
Symptoms You Might Notice
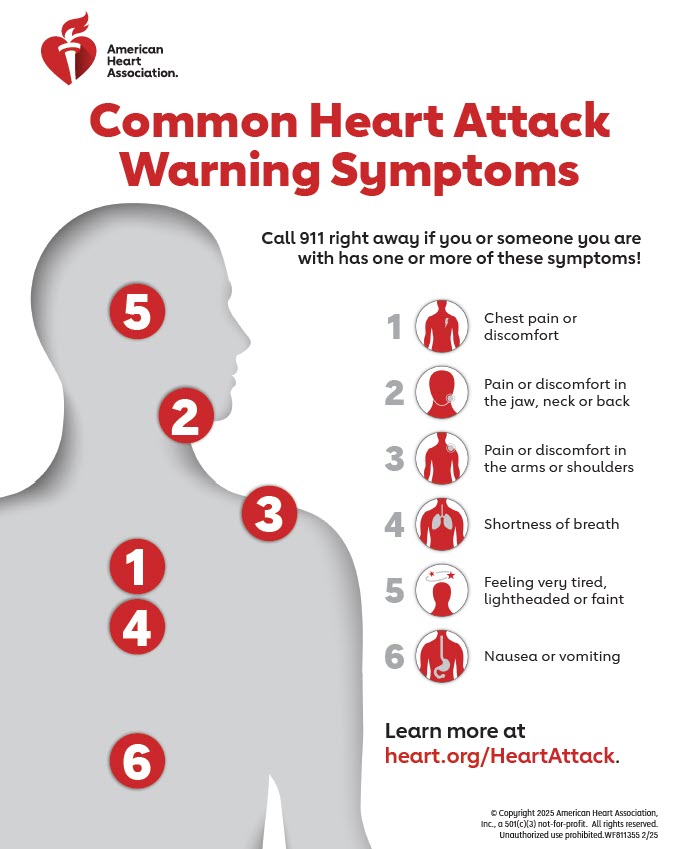
Most folks with a junctional rhythm never feel a thing. The heart is still doing its job, just from a different command center. But when the rhythm slows too much or the underlying cause rattles the system, you might experience:
- Lightheadedness or a faint feeling, especially when standing up quickly
- General fatigue that seems out of proportion to activity
- Occasional palpitationsoften described as a regular thumpthump without the typical flutter
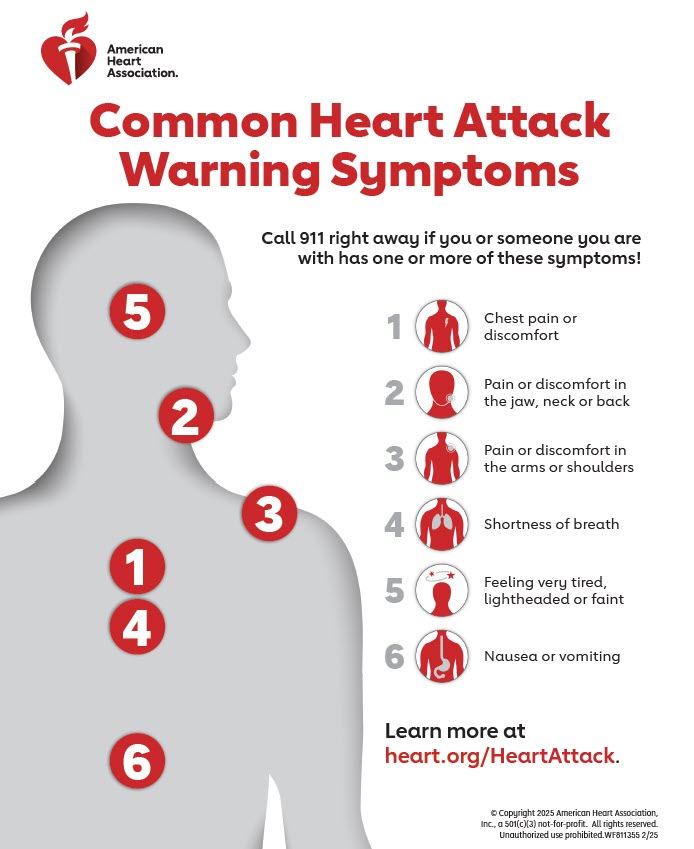
- Chest discomfort, which, if present, should always be evaluated for ischemia
- Rarely, syncope (a brief loss of consciousness) when the rate drops below 40bpm
Think of it like driving a car in a familiar neighborhood but taking a side street you rarely use; you might not notice the change until you hit a pothole (the symptom).
When to Seek Help
If you notice any of the redflag symptomsespecially fainting, chest pain, or a sudden drop in energycall your doctor or head to urgent care. A quick ECG can confirm whether your hearts pacing has shifted and guide the next steps.
ECG Recognition Guide
Reading the Strip
Imagine looking at a musical score; each wave tells a story. In a junctional rhythm, the P wavethe atrial depolarizationoften disappears, or youll see a tiny retrograde P right after the QRS. Heres a quick cheatsheet:
- No P wave: The impulse skips the atria entirely.
- Retrograde P after QRS: The impulse travels backward to the atria.
- Regular rhythm: The intervals between beats stay constant.
- Narrow QRS: Conduction through the ventricles remains normal.
When the rhythm picks up speedsay 7090bpmyoure looking at an accelerated junctional rhythm. Its still regular, but the rate is higher than the classic escape rhythm.
Escape vs. Accelerated: SidebySide
| Feature | Junctional Escape Rhythm | Accelerated Junctional Rhythm |
|---|---|---|
| Rate | 4060bpm | 60100bpm |
| Typical Cause | SAnode failure or suppression | Increased AVnode automaticity (often drugs or mild ischemia) |
| Clinical Outlook | Usually benign, watchful waiting | May hint at underlying irritation; evaluate cause |
When youre discussing this with a clinician, you can say, My ECG shows a regular narrowcomplex rhythm with no P wavescould that be a junctional escape rhythm? That simple sentence shows you understand the basics, which builds trust.
Treatment Options Guide
When No Treatment Is Needed
Most junctional rhythms are like that quiet friend who shows up to a party, doesnt cause any drama, and then quietly leaves. If youre asymptomatic, doctors often recommend:
- Observationrepeat ECG in a few weeks
- Addressing the underlying cause (e.g., adjusting meds, correcting electrolytes)
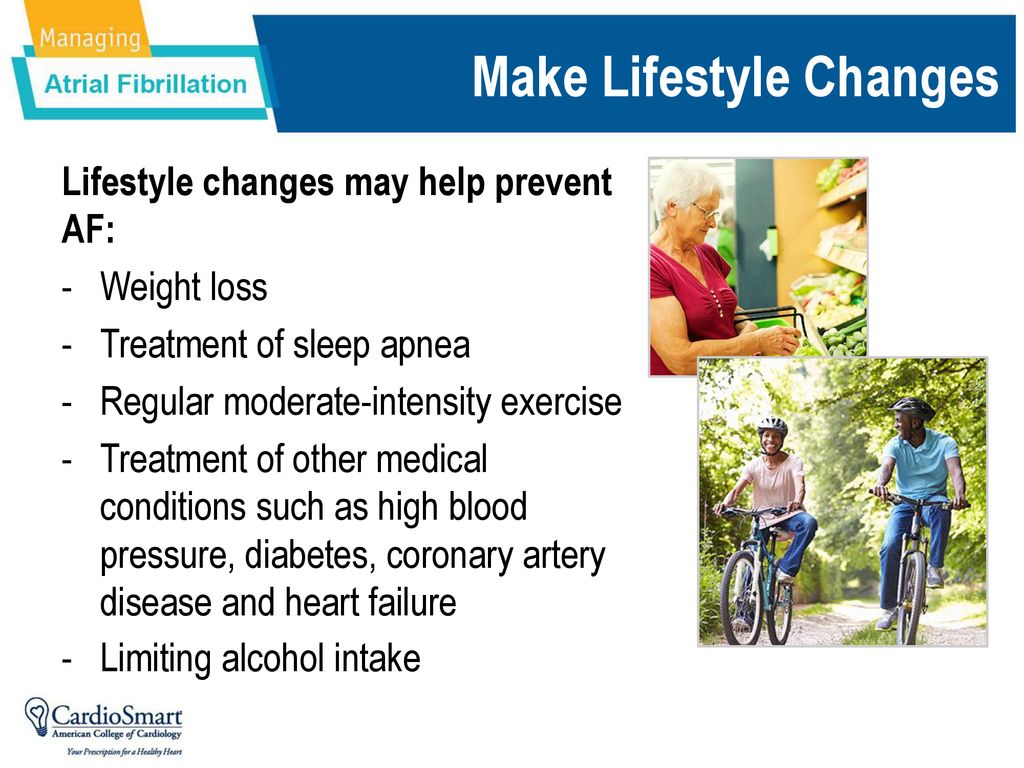
- Lifestyle tweaksstay hydrated, avoid excessive alcohol, manage stress
Think of it as simple housekeeping. You dont need to renovate the whole house if a single light bulb flickers; you just replace the bulb.
Targeting the Root Cause
Because the rhythm is usually a symptom, fixing the trigger is the real cure. Depending on the culprit, you might see:
- Medication adjustment: Lowering the dose of digoxin or betablockers often restores SAnode dominance.
- Electrolyte correction: IV potassium for hypokalemia or dialysis adjustments for hyperkalemia.
- Thyroid management: Levothyroxine for hypothyroidism or antithyroid drugs for hyperthyroidism.
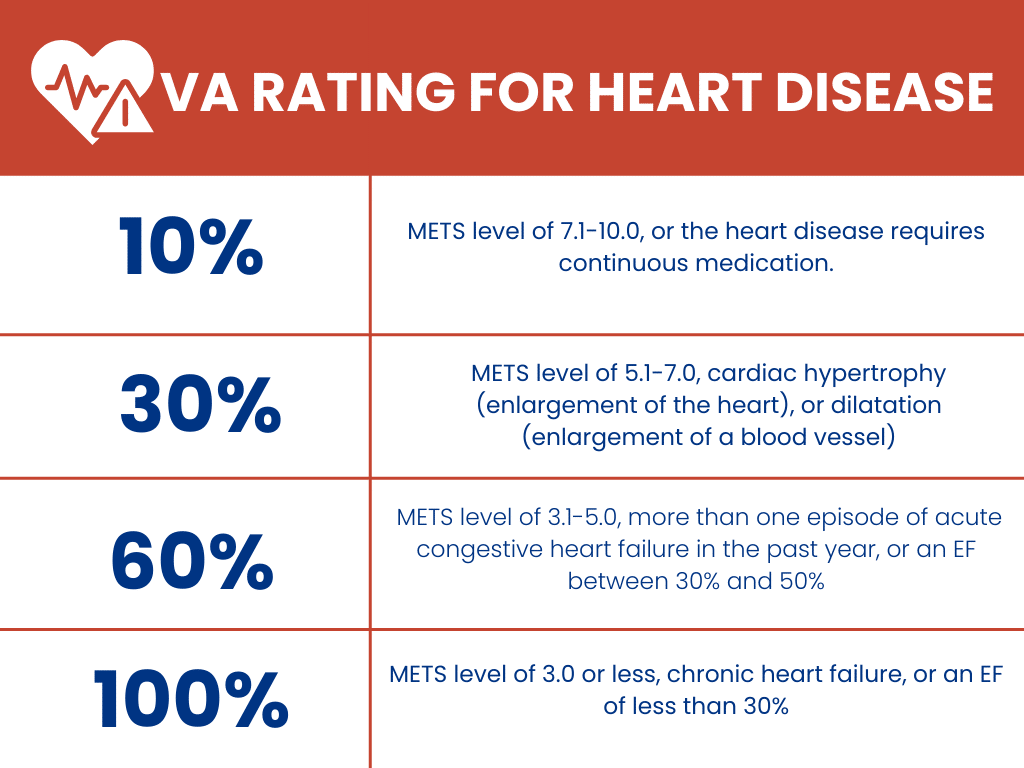
- Ischemia treatment: Revascularization or antiischemic meds if a heart attack is involved.
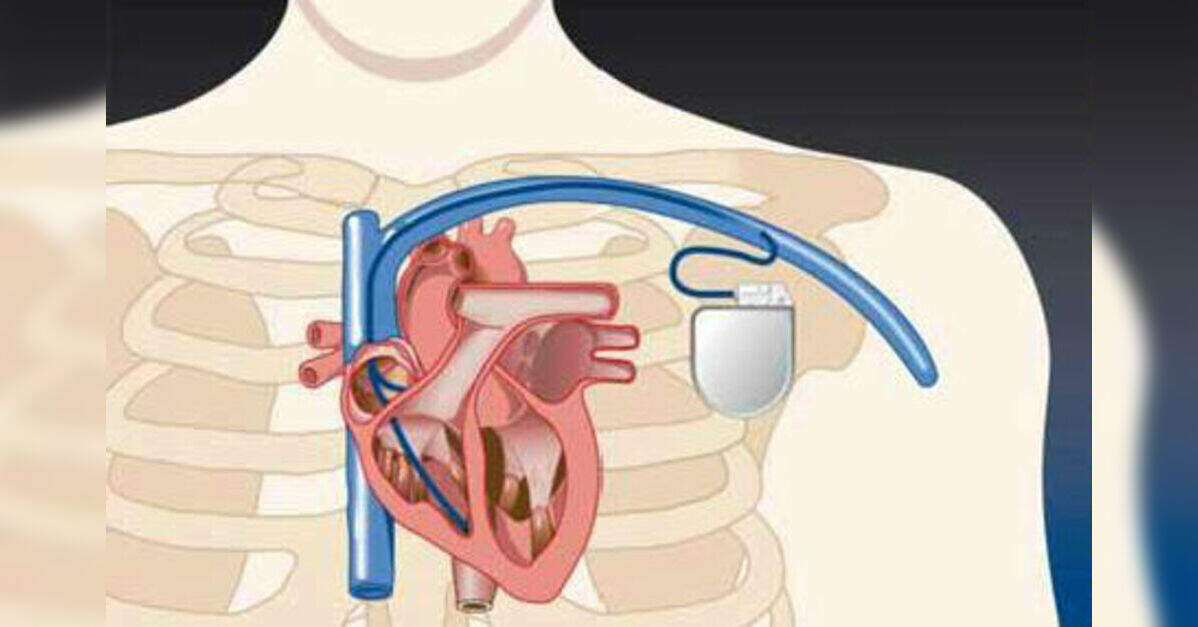
In rare cases where the heart rate is dangerously low and symptoms persist, physicians might reach for or a temporary pacemaker. Those measures are the emergency brake for a runaway situation.
LongTerm FollowUp
Even after the immediate issue is solved, a gentle followup schedule helps ensure the rhythm stays in its sweet spot:
- Repeat ECG or 24hour Holter monitor after 13 months
- Annual checkups if you have chronic conditions (thyroid disease, heart failure)
- Keep a symptom diarynote any dizziness, fatigue, or palpitations and the context (after exercise, medication change, etc.)
Having a record is like keeping a logbook for a car; it tells the mechanic (your doctor) exactly when something changed. If you have signs of fluid overload or leg swelling while dealing with arrhythmias, evaluating leg swelling cause can help uncover contributing problems such as heart failure or edema.
RealWorld Cases
Case Study 1: PostSurgery Switch
Mark, a 62yearold retired teacher, underwent coronary artery bypass grafting. Two days postop, his bedside monitor showed a steady rate of 48bpm with no visible P waves. The cardiology team diagnosed a junctional escape rhythm, likely from intraoperative trauma to the SA node. They held off on any medication changes, simply monitored him, and the rhythm reverted to normal sinus after five days as the tissue healed.
Case Study 2: MedicationInduced Acceleration
Lisa, 45, was started on digoxin for atrial fibrillation. During a routine followup, her ECG revealed a regular 78bpm rhythm with absent P wavesclassic for an accelerated junctional rhythm. The doctor reduced her digoxin dose and added a lowdose betablocker to control rate. Within a week, her ECG returned to normal sinus rhythm, and she felt less fluttery.
Both stories illustrate the balance between watchful waiting and targeted intervention. They also show why sharing your medication list and recent surgeries with your doctor can make all the difference.
Bottom Line
A junctional rhythm is essentially your hearts builtin backup planusually harmless, sometimes a signal that something else needs attention. By learning its telltale ECG clues, recognizing common causes, and understanding when to simply observe versus when to act, you empower yourself to stay on top of heart health.
If any of this resonated with you, or if youve experienced an unexpected rhythm change, lets keep the conversation going. Share your story in the comments, ask any lingering questions, or simply give this article a thumbsup if it helped you feel a bit more at ease. Your heart beats for youlets make sure you understand its rhythm together.
FAQs
What is a junctional rhythm?
A junctional rhythm is an arrhythmia where the electrical impulse that normally starts in the sino‑atrial (SA) node instead originates from the atrioventricular (AV) node or His bundle, acting as the heart’s backup pacemaker.
How can I identify a junctional rhythm on an ECG?
On an ECG you’ll see a regular, narrow‑complex rhythm with absent, inverted, or retrograde P waves that may appear hidden within or just after the QRS complexes. The rate is usually 40‑60 bpm (escape) or 60‑100 bpm (accelerated).
What are the most common causes of a junctional rhythm?
Typical triggers include SA‑node suppression from medications (e.g., digoxin, beta‑blockers), myocardial infarction, electrolyte imbalances (especially potassium), thyroid disorders, postoperative changes after cardiac surgery, and inflammatory heart conditions such as myocarditis.
When does a junctional rhythm require treatment?
If you are asymptomatic, observation and correction of the underlying cause are usually enough. Treatment becomes necessary when the rate is dangerously low, symptoms like dizziness or syncope occur, or the rhythm is caused by a reversible but acute issue that needs immediate correction (e.g., severe hyper‑kalemia).
What symptoms should prompt me to seek medical care?
Red‑flag symptoms include sudden fainting, persistent light‑headedness, chest pain, palpitations, or a noticeable drop in exercise tolerance. Any of these warrant prompt evaluation and an ECG.