By the time you hit the sixmonth mark after an aortic valve replacement, most folks are feeling a lot more like themselves againbut a few lingering symptoms can still pop up. Shortness of breath, occasional chest discomfort, or a lingering sense of fatigue arent uncommon, and knowing whats normal versus what needs a doctors eye can make all the difference.
In this article well walk through the typical milestones you can expect, flag the warning signs you shouldnt ignore, share diet and activity tips, compare your progress to earlier and later checkpoints, and sprinkle in realworld stories so you dont feel alone on this journey. Grab a cup of tea, settle in, and lets talk about life six months after aortic valve replacement.
Typical SixMonth Milestones
Can I return to work, exercise, and social life?
Most patients find they can resume regular work and light to moderate exercise around the threemonth point, and by six months many are back to fulltime jobs and social outings. The key is a gradual rampup: start with short walks, then add a light jog or a gentle bike ride, and finally incorporate strength training with light weights.
Think of your recovery like building a sandcastlelayer by layer. If you try to stack the whole thing in one go, it collapses. But if you add one sturdy layer at a time, the structure holds up beautifully.
Heres a quick timeline you might recognize:
| Time Frame | Typical Activities |
|---|---|
| 04 weeks | Rest, short walks, breathing exercises |
| 13 months | Increasing walking distance, light housework |
| 36 months | Jogging, swimming, returning to office work |
| 6+ months | Full gym routine, hobbies, travel |
Which symptoms are still normal at this stage?
Its perfectly okay to feel a little winded after climbing a flight of stairs or to notice a faint ache around the sternum when you first get up in the morning. Studies from the American Heart Association show that up to 30% of patients report mild shortness of breath , and this usually eases as your heart remodels around the new valve.
Common normal sensations include:
- Occasional chest soreness that improves with movement.
- Light fatigue after a busy day, especially if youre still building stamina.
- Minor irregular beats (premature beats) that feel like a hiccup in your heart rhythm.
If these symptoms are mild, dont panicjust keep a symptom diary and share it with your cardiologist at your next visit.
How does mental health usually evolve?
Recovering from openheart surgery isnt just a physical feat; its an emotional marathon, too. Research published in the Journal of Cardiovascular Nursing found that anxiety scores drop by roughly three points between three and six months postop, thanks to increased confidence in daily activities.
That said, its natural to feel a bit on edge when youre still adjusting to a new rhythm. Simple practices like daily mindfulness, short breathing exercises, or joining a local heartpatient support group can make a world of difference. Trust me, sharing a cup of coffee with someone whos been through the same screwdriversized chest incision can be surprisingly comforting.
RedFlag Warning Signs
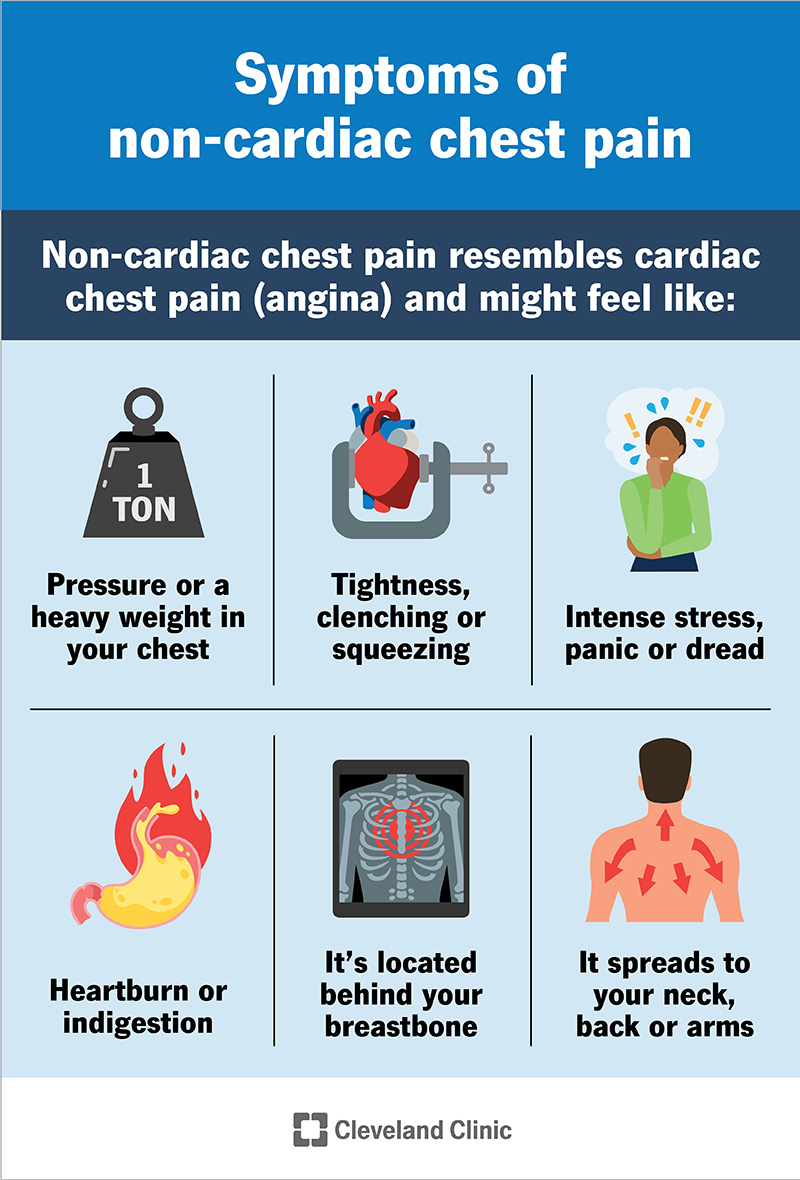
Chest pain months after aortic valve replacement
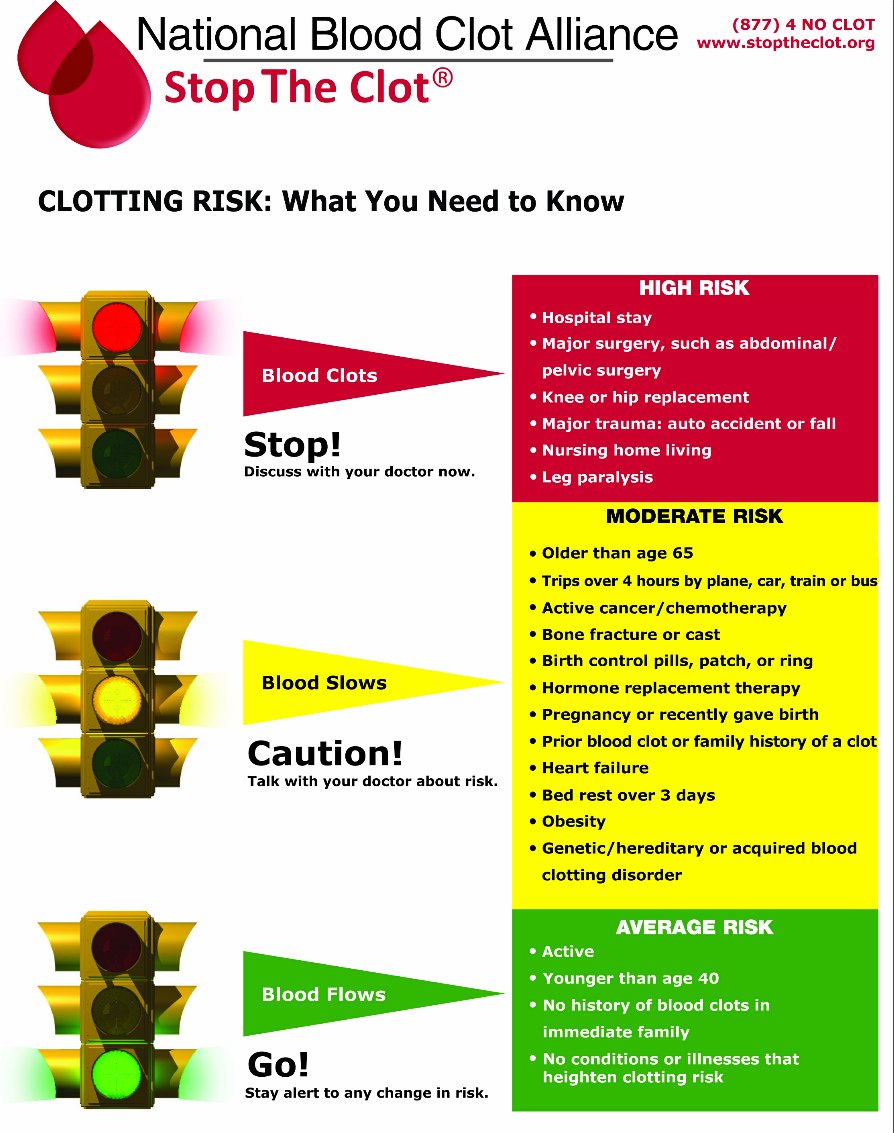
Postsurgical pain usually fades within weeks. If you notice a sharp, burning, or pressurelike sensation that lasts more than a few minutes, especially if it spreads to your arm, jaw, or back, treat it as a red flag. This could signal valve dysfunction, infection, or a new cardiac issue.
Ask yourself:
- Is the pain sudden or gradual?
- Does it worsen with activity or deep breaths?
- Is it accompanied by sweating, nausea, or dizziness?
If you answer yes to any of these, call your cardiac surgeon or head to the emergency department right away.
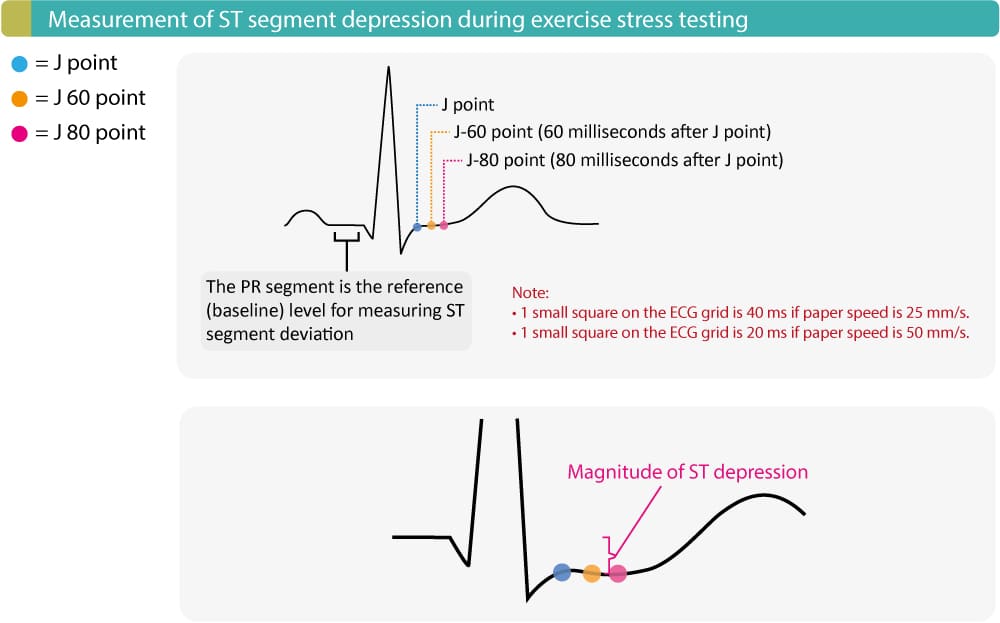
Sudden shortness of breath or worsening fatigue
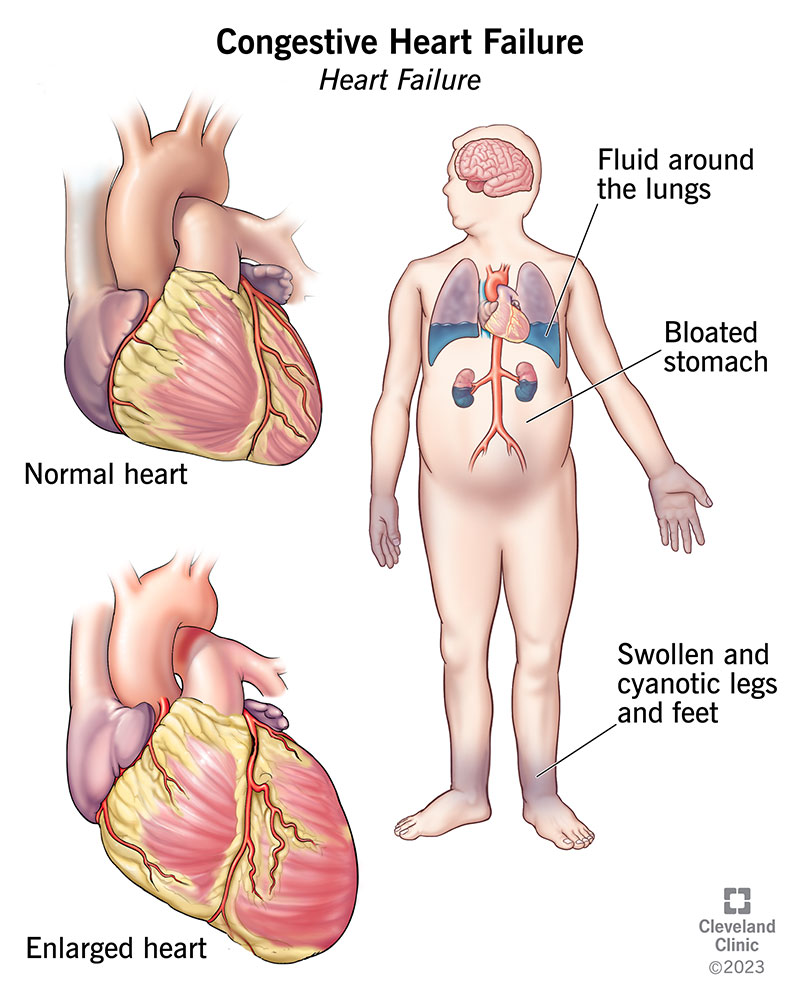
While a bit of breathlessness is normal, a sudden increase in breathlessnessor fatigue that feels out of proportion to your activity levelmight hint at valve leakage, arrhythmia, or even pulmonary edema.
Try the SABQ selfcheck:
- Severity: Is it mild, moderate, or severe?
- Activity: Does it happen at rest or only with exertion?
- Breathing: Are you gasping for air or just a little winded?
- Quality: Is the sensation sharp, dull, or heavy?
If the answers point toward moderatetosevere or it happens at rest, reach out to your heart team immediately.
Signs of infection or valve degeneration
Infections can sneak up quietly. Fever, night sweats, unexplained chills, or a new heart murmur on your routine exam deserve prompt evaluation. Longterm complications after aortic valve replacement, such as prosthetic valve endocarditis, are rare but serious.
Keep an eye on:
- Temperature over 100.4F (38C)
- Persistent coughing, especially with sputum
- Redness or drainage at the incision site (even months later)
When in doubt, call your cardiologistbetter safe than sorry.
Lifestyle Nutrition Guidance
Foods to avoid after heart valve replacement
Nutrition plays a starring role in keeping your new valve happy. If youre on blood thinners, highsodium foods and vitaminKrich items (like kale, spinach, and broccoli) can mess with your INR levels. Also, raw or undercooked fish should be avoided if you have a mechanical valve to reduce infection risk.
Heres a quick doanddont list:
| Do | Dont |
|---|---|
| Choose fresh fruits, steamed veggies, lean proteins. | Eat processed meats, salty snack foods. |
| Use herbs and spices for flavor instead of salt. | Consume large amounts of leafy greens if on warfarin without monitoring. |
| Stay hydratedaim for 8 cups of water daily. | Drink excessive alcohol (it interferes with anticoagulants). |
Exercise recommendations for the 6month window
By six months youre ready for a balanced routine:
- Cardio: 30 minutes of moderateintensity activity (brisk walking, cycling, swimming) at least five days a week.
- Strength: Light resistance trainingthink 23 sets of 1012 reps with dumbbells or resistance bands, twice weekly.
- Flexibility: Gentle stretching or yoga sessions to improve chest wall mobility.
Check your exertion using the talk test: you should be able to hold a conversation without gasping. If you own a smartwatch, keep an eye on your heart rateaim for 5070% of your agepredicted max during cardio.
Managing fatigue after openheart surgery
Fatigue six months postop can feel like youre dragging a sack of bricks around. The good news? Its usually a mix of deconditioning and the body still healing.
Try these tricks:
- Prioritize sleep hygienedark room, cool temperature, no screens an hour before bed.
- Break tasks into smaller chunks; use pacing (workrestwork) to conserve energy.
- Stay hydrated and keep a balanced snack handy (protein + carbs) to avoid energy crashes.
Most patients notice a steady climb in energy levels after they lock into a consistent routine.
Comparing Time Points
3 months after aortic valve replacement
At three months, many patients are still testing the watersshort walks, easing back into work, and dealing with occasional sternum pain. The hearts remodeling process is in full swing, and the risk of early complications is higher than at six months.
1 year after aortic valve replacement
By the oneyear mark, the majority have achieved a new normal. Echo studies often show optimal valve function, and exercise tolerance usually matches or exceeds presurgery levels. Longterm complications become rarer, though annual checkups remain essential.
6 months after mitral valve replacement
If youve had a mitral valve replacement instead, the recovery timeline is similar, but you might notice slightly different symptom patternssuch as more noticeable shortness of breath when lying flat, due to the leftright blood flow dynamics. Nonetheless, the same milestones and redflag signs apply.
Expert Guidance Evidence
Key clinical guidelines
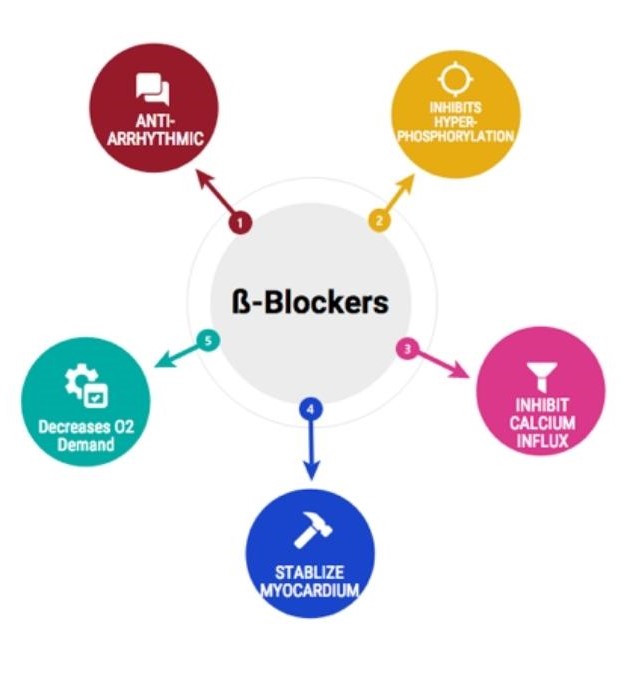
The 2024 ACC/AHA valvereplacement guidelines recommend a routine echocardiogram at six months, blood work to check anticoagulation levels (if applicable), and a structured cardiac rehabilitation program. Following these protocols dramatically reduces the odds of late complications.
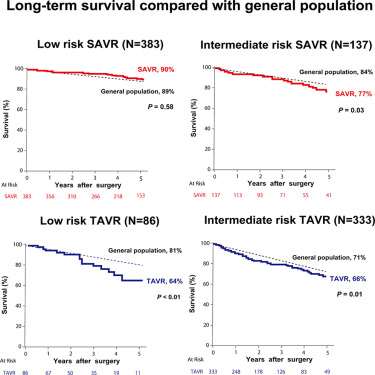
Recent studies
According to a 2024 study in Circulation, patients who adhered to a supervised rehab program saw a 25% faster return to baseline functional capacity compared with those who exercised on their own. Another paper in the Journal of Thoracic Surgery highlighted that fatigue scores improve most dramatically between the third and sixth month after surgery.
When to schedule your next cardiology appointment
Plan for:
- A sixmonth echocardiogram to confirm valve performance.
- Lab work for INR (if on warfarin) or other anticoagulants.
- A medication reviewdosage tweaks are common as your body stabilizes.
- Discussion of any lingering symptoms (chest pain, shortness of breath, fatigue).
Patient Stories Experience
Ruths 6month journey
Ruth, a 58yearold teacher from Seattle, shared that she was back in the classroom by week 12, but at six months she still felt a tightness when climbing her stairs. A quick echo showed her valve working perfectly; the sensation was actually mild muscle strain from returning to a standingdesk routine. With a physiotherapists help, she cleared the issue within weeks.
Typical day in the life of a 6month postop patient
Imagine a weekday:
- 7:00am Morning meds, light stretching.
- 8:00am 30minute brisk walk while listening to a podcast.
- 9:30am Back to work (virtual meetings, standing desk).
- 12:30pm Light lunch (grilled chicken salad, lowsodium dressing).
- 3:00pm Short break for deepbreathing exercises.
- 5:30pm Gentle yoga session, focusing on chest opening.
- 7:00pm Dinner with omega3rich fish, steamed veggies.
- 9:30pm Relax, read, and head to bed by 10pm.
This rhythm blends activity with rest, keeping the heart and mind happy.
FAQstyle poll from a heartpatient forum
When asked What symptom worried me the most at six months? the top answer was intermittent chest pressure after climbing stairs. The consensus advice: track the episodes, note intensity and duration, and bring the log to your next cardiology visit.
Practical Tools Takeaways
Checklist: Am I on track at 6 months?
Downloadable PDF (link placeholder) includes items like Can I walk 30 minutes without stopping? and Do I need to adjust my medication? Use it to stay organized and proactive.
Symptomtracker template
Keep a simple table in your phone or notebook to record any chest pain, shortness of breath, or fatigue episodes. Share this with your doctor for a clearer picture of your recovery curve.
Quickreference diet guide
Print out the Foods to Avoid table above and stick it on your fridge. A visual reminder can make healthy choices feel like second nature.
Remember, six months after aortic valve replacement is a milestoneone that blends triumph with a few lingering questions. Embrace the progress youve made, stay vigilant for any redflag signs, and lean on the support of your medical team, friends, and family. Your heart has taken a big step; now its time for you to take the next confident one.
Whats been your biggest win or challenge at the sixmonth mark? Share your story in the comments, or drop a line if you have any lingering questions. Were in this together.
If youre tracking persistent swelling or fluid retention as part of your recovery, consider learning more about heart failure edema and its management to discuss symptoms with your cardiology team.
FAQs
What types of exercise are recommended at the six‑month mark?
Moderate‑intensity cardio (e.g., brisk walking, cycling, swimming) for 30 minutes most days, light resistance training 2–3 times per week, and gentle stretching or yoga to keep the chest wall mobile.
Is it normal to feel shortness of breath after climbing stairs?
Yes, a mild breathlessness after a flight of stairs is common at six months. It usually improves as stamina builds, but if it becomes severe or occurs at rest, contact your cardiologist.
When should I be concerned about chest pain?
Sharp, burning, or pressure‑like chest pain that lasts more than a few minutes, spreads to the arm, jaw, or back, or is accompanied by sweating, nausea, or dizziness requires immediate medical attention.
What foods should I limit if I’m on a blood thinner?
Avoid high‑sodium processed foods and large amounts of vitamin K‑rich vegetables (e.g., kale, spinach) unless your INR is monitored. Also steer clear of raw or undercooked fish if you have a mechanical valve.
How often should I see my cardiologist after six months?
Schedule a routine follow‑up that includes a six‑month echocardiogram, INR or anticoagulant labs if applicable, medication review, and a discussion of any lingering symptoms.