Wondering how soon you'll be able to breathe easily after a nose job? In most cases, you'll start feeling a difference within a couple of weeks, but the true normal can take a few months as swelling fades and tissues settle. Below you'll find a friendly, down-to-earth guide that walks you through every stage, highlights the red flags, and gives you practical tips to keep the air flowing.
Immediate Post-Op
Why Swelling Blocks Airflow
After your surgeon reshapes cartilage or bone, the lining of the nose (the mucosa) gets a little puffy. Think of it like a garden hose that's been squeezedwater can't move freely. This swelling is completely normal and usually peaks within the first 35 days.
Timeline of Swelling Reduction
| Days Post-Surgery | What You'll Feel |
|---|---|
| 07 | Heavy congestion, frequent mouth-breathing, possible use of nasal splints. |
| 821 | Swelling starts to recede; nasal strips or a saline rinse can help. |
| 2284 | Most patients can breathe through the nose most of the day. |
| 36 months | Final tissue remodeling; breathing should feel normal. |
Typical Symptoms You'll Notice
It's common to feel blocked or to slip into mouth breathing after rhinoplasty. The key is distinguishing temporary irritation from a problem that needs a doctor's eye. If you can clear secretions with a gentle blow or a saline rinse, you're likely in the normal healing window.
Red-Flag Symptoms
Persistent blockage beyond six months, severe pain, or any uncontrolled bleeding should prompt a quick call to your surgeon. A post-op checkup can rule out scar tissue, infection, or a structural issue that might need a minor revision.
Recovery Factors
Surgical Scope Matters
When the procedure includes a septoplasty (straightening the septum) alongside the cosmetic changes, many patients report a faster return to easy breathing. The reason? The surgeon is already addressing the internal wall that often causes chronic congestion.
Impact of Combined Septorhinoplasty
Studies from the field show that patients who receive both cosmetic reshaping and septal correction have a 30% higher satisfaction rate regarding airflow.
Patient-Specific Variables
Your age, smoking status, and any pre-existing allergies can lengthen or shorten the healing curve. A smoker's lungs already struggle with irritation, so the nasal tissues take longer to calm down. Likewise, if you've had a deviated septum for years, you might notice a bigger improvement once that piece of cartilage is set straight.
Post-Op Care That Helps
- Use a saline spray 34 times daily to keep the lining moist.
- Elevate your head while sleeping for the first two weeks.
- Avoid heavy lifting or intense cardio for at least three weeks.
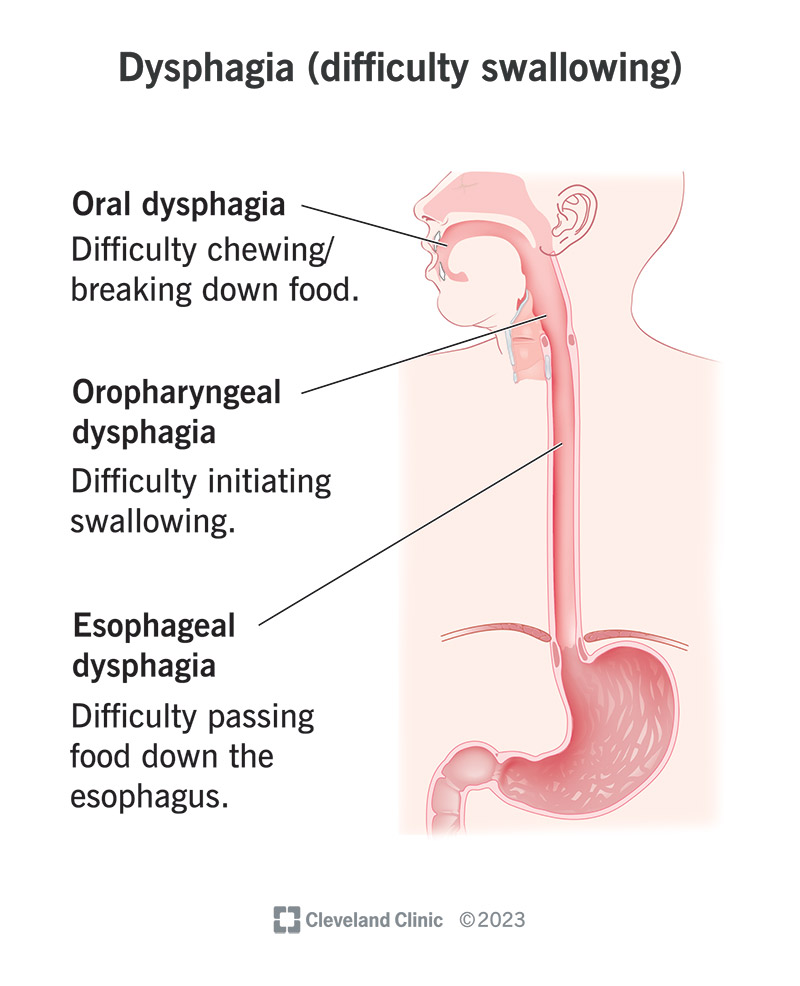
- If you're prone to allergies, discuss a short course of antihistamines with your doctor. For those also experiencing dysphagia causes, always consult your physician for a comprehensive evaluation.
Persistent Issues
When Breathing Problems Stick Around
Most lingering issues fall into two camps: functional (the nose isn't physically open enough) or inflammatory (excess scar tissue). A common cause is over-resection of cartilage, which can weaken the nasal valvethe narrowest part of the airway.
What Reddit Users Say
Scrolling through r/rhinoplasty you'll find threads titled "mouth breathing after rhinoplasty" where people share their frustrations. Many describe a "mushy" feeling weeks after surgery. The consensus? If the problem persists past six weeks, schedule a check-up appointment.
Blocked Nose Six Months After Surgery
A blocked nose half a year out isn't normal. It could signal scar tissue buildup or an unseen deviation that was missed the first time. An ENT specialist can perform a nasal endoscopy to pinpoint the causeoften a quick in-office procedure.
When to Consider Revision
If the obstruction is structural, a minor revision (sometimes called a functional rhinoplasty) can restore the airway without dramatically changing the aesthetic result. Insurance may cover part of the cost if the surgery is deemed medically necessary.
Managing Breathing
At-Home Remedies That Actually Work
Here are a few simple tricks you can try right now:
- Steam inhalation: A bowl of hot water with a towel over your head loosens mucus.
- Humidifier: Adding moisture to bedroom air reduces dryness that can aggravate the lining.
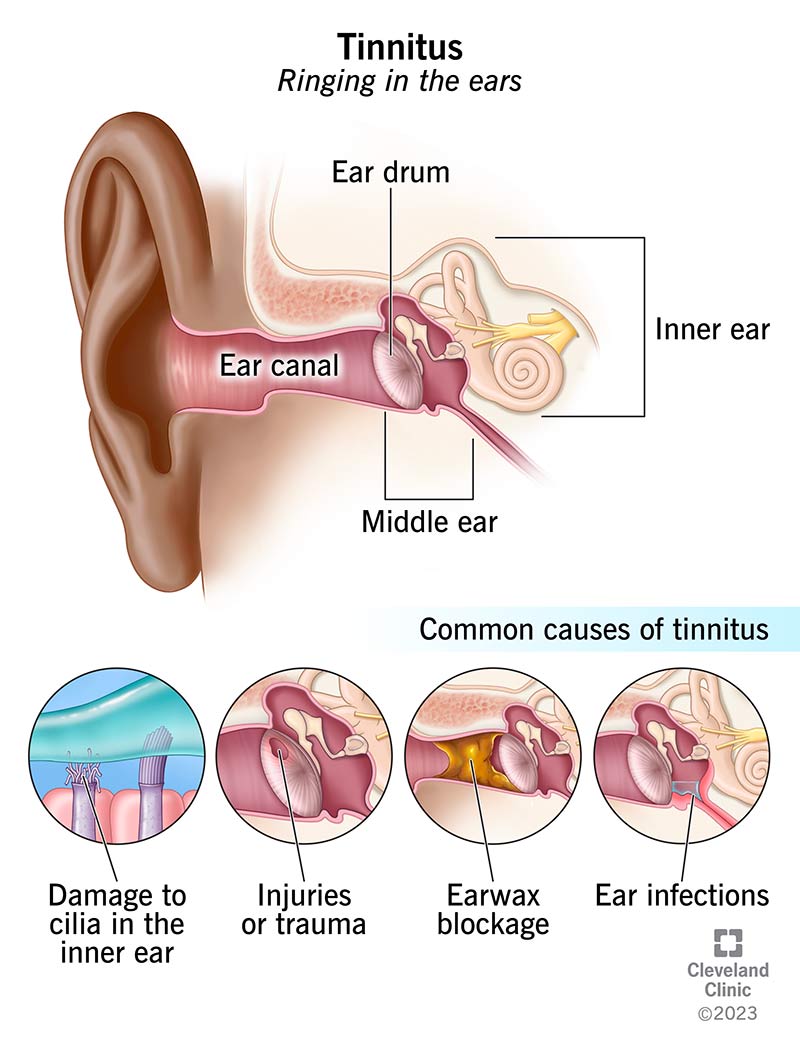
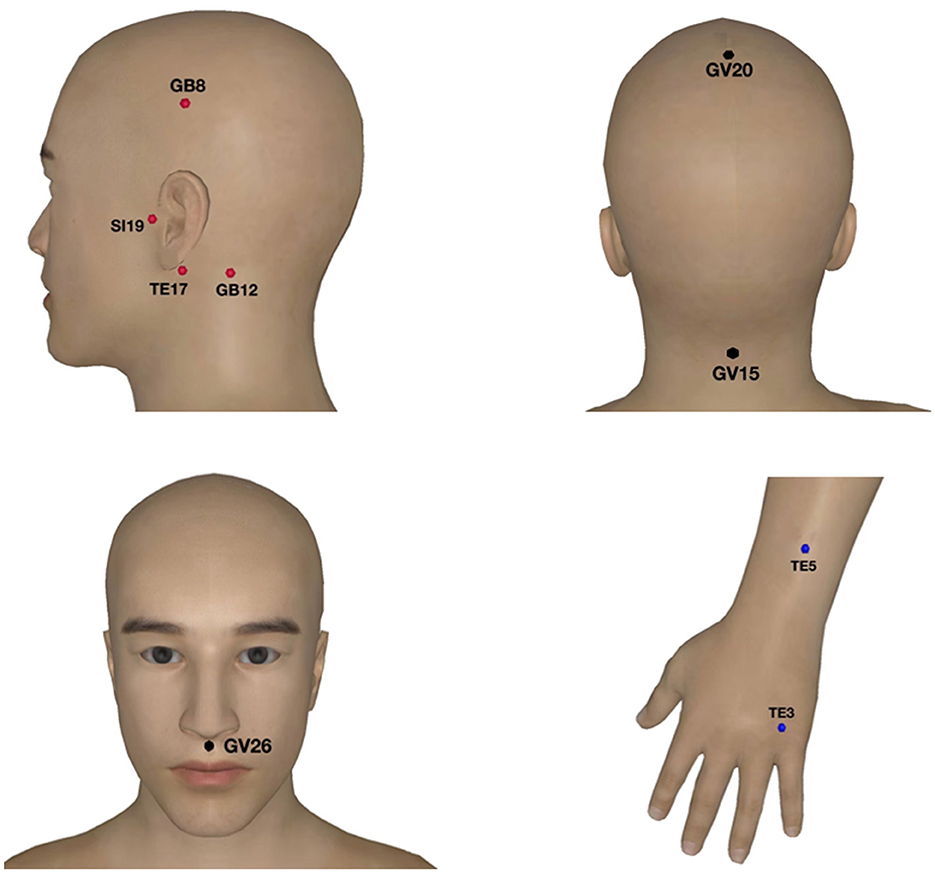
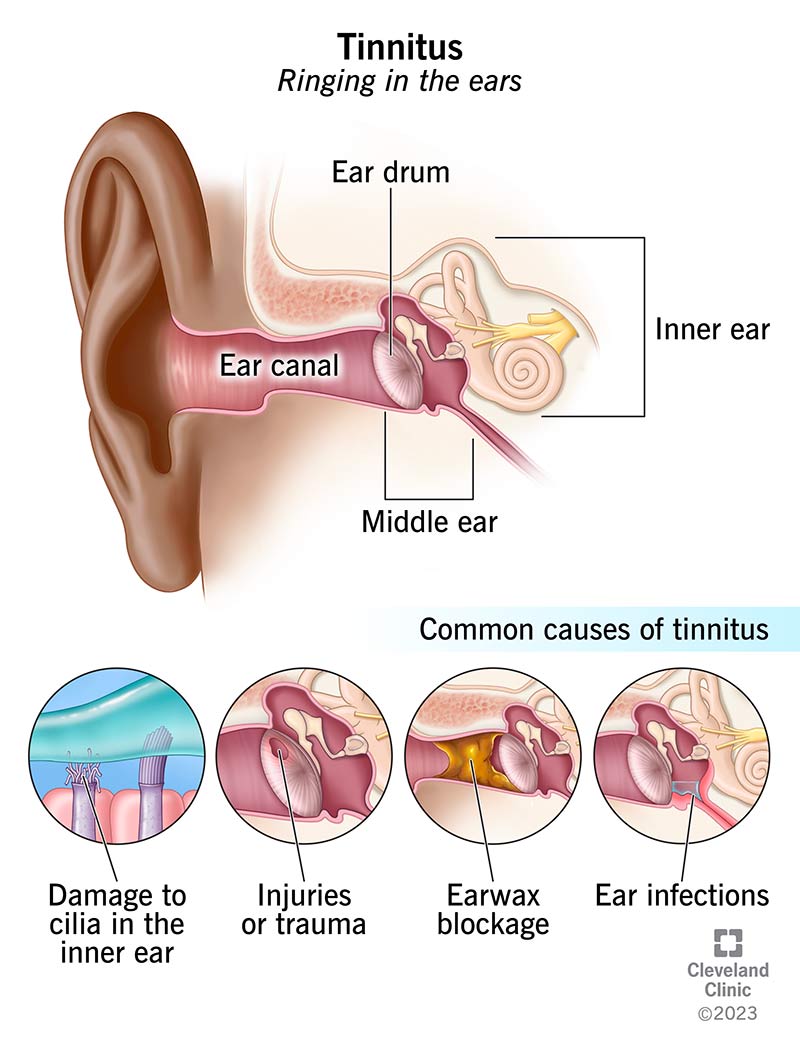
- Breathing exercises: The box breathing technique (inhale 4s, hold 4s, exhale 4s, hold 4s) encourages nasal airflow. Some patients also find relief through complementary therapies such as yoga for tinnitus, which can help with relaxation and improve overall respiratory habits.
When to Call Your Surgeon
Make a note of these signs and give your surgeon a ring if any appear:
- Fever over 38C (100.4F).
- Severe facial pain that isn't relieved by prescribed meds.
- Bleeding that won't stop after 15 minutes of gentle pressure.
- Worsening congestion after the 3-week mark.
Medical Interventions
If home care isn't enough, a doctor might suggest:
- Prescription nasal steroid sprays to shrink lingering inflammation.
- Temporary internal splints that support the nasal valve.
- In rare cases, a minor revision surgery focusing on the valve or scar tissue.
Cost Considerations
Wondering about the price tag? Here's a quick snapshot of typical costs in the United States (all figures are averages and can vary by region and surgeon experience):
| Procedure | Average Cost | Insurance Coverage? |
|---|---|---|
| Cosmetic Rhinoplasty | $8,000 $12,000 | No |
| Septoplasty (functional only) | $4,000 $7,000 | Often yes |
| Combined Septorhinoplasty | $9,000 $15,000 | Partial, if deemed medically necessary |
Expert Insights
What Surgeons Recommend
Dr. Saigal, a board-certified facial plastic surgeon, says, "Patients should expect noticeable swelling for the first 23 weeks, but true respiratory improvement often isn't fully apparent until the 3-month mark." He also stresses the importance of a thorough pre-op conversation about breathing goals, not just aesthetics.
Data From Peer-Reviewed Studies
A 2023 meta-analysis in the Aesthetic Surgery Journal reported a 92% success rate for functional improvement when rhinoplasty included septal correction. The same study warned that over-aggressive cartilage removal could increase the risk of long-term nasal valve collapse.
Choosing the Right Surgeon
Look for these credentials before signing the consent form:
- Board certification in facial plastic surgery or otolaryngology.
- At least 150 completed rhinoplasty cases, with a sizable portion involving functional correction.
- Positive before-and-after galleries that show both aesthetic and airway outcomes.
Building Trust
Transparency matters. A reputable surgeon will share realistic before-and-after photos, discuss potential complications, and outline a clear post-op plan. If they can't provide references or clear answers, keep looking.
Common Questions
How long does it take for breathing to be normal after rhinoplasty?
Most patients notice a substantial improvement within 46 weeks, but the final "normal"where swelling has fully resolvedusually arrives between 36 months.
Can rhinoplasty make my breathing worse?
Yes, if too much cartilage is removed or the nasal valve is unintentionally narrowed. That's why many surgeons combine a functional septorhinoplasty to protect the airway.
Is mouth breathing after rhinoplasty normal?
A mild increase in mouth breathing is typical for the first 23 weeks while the nose is still swollen. If it continues beyond 6 weeks, it's worth an evaluation.
Do I need a septoplasty to fix breathing?
If a deviated septum contributes to the blockage, a septoplasty (often done at the same time as the cosmetic work) is the most effective solution.
What is the cost of a functional rhinoplasty?
In the U.S., a combined functional-cosmetic procedure runs roughly $9,000$15,000. Insurance may cover part of the cost when the surgery is deemed medically necessary for breathing.
Conclusion
Breathing after a nose job is a journeyone that starts with a little swelling and ends with clearer, easier airflow. By understanding the typical timeline, recognizing the signs that call for a doctor's eye, and giving your body the right aftercare, you set yourself up for a smooth recovery. If you've experienced any of the challenges mentioned here, don't hesitate to reach out to your surgeon or share your story in the comments. Your experience might help the next person feeling unsure about their own breathing after rhinoplasty.
FAQs
How long does it take to breathe normally after rhinoplasty?
Most patients notice a significant improvement within 4‑6 weeks, but the final “normal” breathing usually settles between 3‑6 months as swelling fully resolves.
Can rhinoplasty make my breathing worse?
Yes, if too much cartilage is removed or the nasal valve is unintentionally narrowed. Combining the procedure with a septoplasty reduces this risk.
What red‑flag symptoms should prompt a call to my surgeon?
Persistent blockage beyond six months, severe facial pain, uncontrolled bleeding, fever over 38 °C (100.4 °F), or worsening congestion after the 3‑week mark require immediate evaluation.
Does adding a septoplasty improve breathing after rhinoplasty?
When a deviated septum is corrected during the same surgery, many patients experience faster and greater improvement in airflow, with higher satisfaction rates.
When is a revision surgery needed for breathing issues?
If obstruction persists past six weeks and is due to structural problems like nasal valve collapse or scar tissue, a minor functional revision may be recommended.