Quick Answer Overview
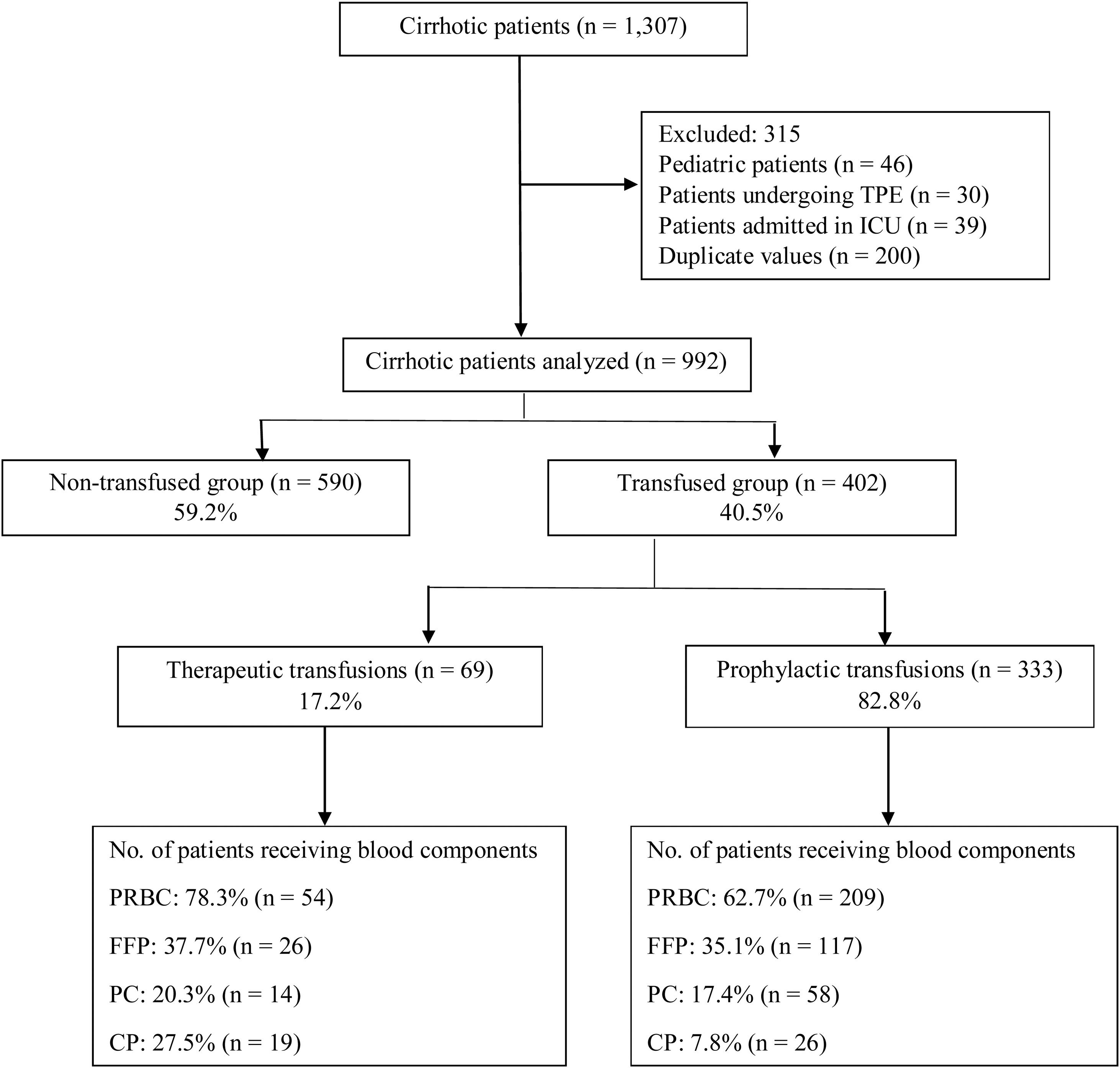
If you or a loved one has cirrhosis and a low platelet count, you might wonder whether a platelet transfusion is the right move. In short, platelet transfusion in cirrhosis is a targeted rescue when the platelet count drops below a safe threshold (usually under 5010/L) and a medical procedure or bleeding risk is looming. It's not a routine give-it-anyway treatment; doctors weigh the benefits against the possible complications before pulling the trigger.
Bottom line: most people with cirrhosis can avoid transfusions by planning procedures carefully, using newer medications that boost platelets, and making lifestyle tweaks. But when the bleeding risk is high, a well-timed transfusion can be a lifesaver.
Why Platelets Drop
How Liver Failure Affects Production
The liver makes a hormone called thrombopoietin (TPO) that tells bone marrow to crank out platelets. When the liver is scarred, its TPO output dwindles, so fewer platelets are released into the bloodstream. Imagine a factory losing its manager production slows down, right?
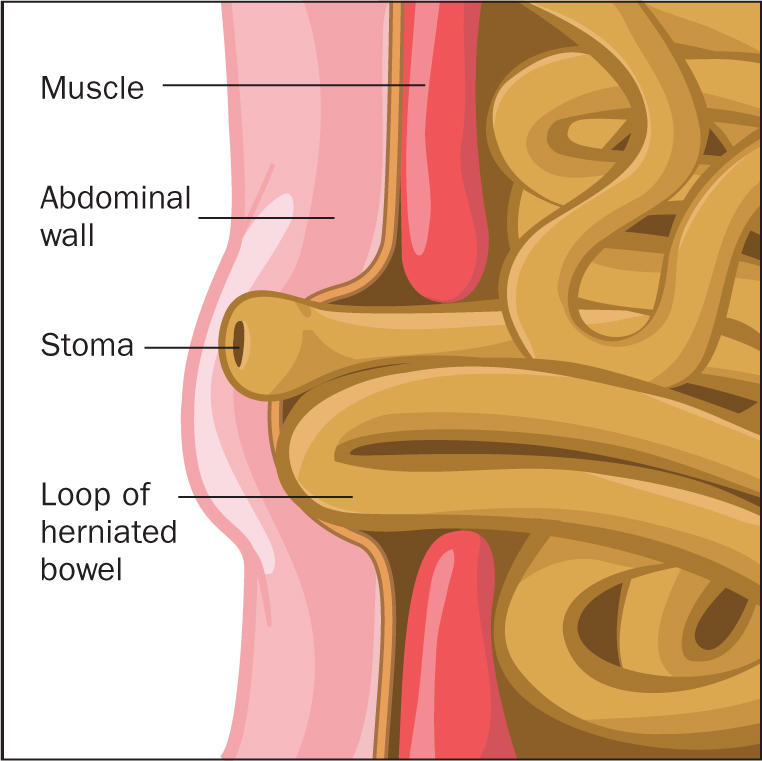
The Role of Hypersplenism
Advanced cirrhosis often brings an enlarged spleen (splenomegaly). The spleen acts like a storage closet that hoards about a third of the body's platelets. When it swells, it grabs even more, leaving the circulation shortchanged. This splenic sequestration explains why many patients with end-stage liver disease have a low platelet count even when bone marrow function is okay.
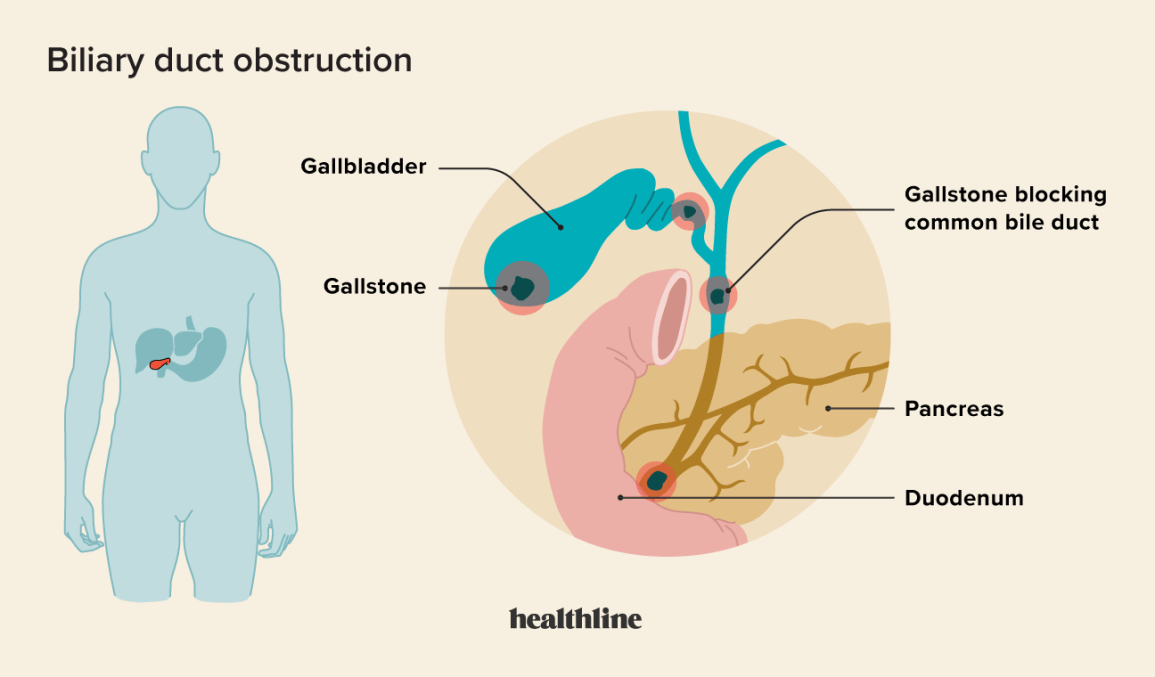
Why Liver-Failure Patients Need Blood Transfusions
Beyond platelets, cirrhosis can cause coagulopathy (problems with clotting factors) and fragile blood vessels, especially in the esophagus and stomach. Those varices can bleed catastrophically, and a sudden drop in platelets makes the situation worse. That's why doctors sometimes give transfusions before high-risk procedures.
Real-World Example
John, a 58-year-old who's been battling alcoholic liver disease for a decade, was scheduled for an upper endoscopy to check his varices. His platelet count had slipped to 4210/L. His hepatologist explained the risks and decided to give a single platelet unit right before the scope. The procedure went smoothly, and John left the hospital without a bleed. A few weeks later, with better nutrition and a TPO-receptor agonist, his platelet count stayed above 8010/L, and no further transfusions were needed. For nutritional support and lifestyle modifications in liver-related conditions, consider learning more about ulcerative colitis supplements which can support overall digestive health.
When to Transfuse
Standard Thresholds
Most guidelines suggest a platelet count of 5010/L for routine invasive procedures (like liver biopsy or paracentesis). For high-risk endoscopic work, some centers aim for 3010/L. Below those numbers, the bleeding odds rise noticeably.
Liberal vs. Restrictive Strategies
There's an ongoing debate: should we give platelets liberally to keep numbers nice and high, or should we be more conservative? A 2023 study in the American Journal of Medicine found that a liberal approach reduced minor bleeding but didn't affect major outcomes, while a 2022 paper in World Journal of Gastroenterology showed that a restrictive strategy cut down on transfusion-related complications without raising serious bleed rates. The takeaway? Tailor the plan to the patient's overall health, not just the platelet count.
Procedures That Usually Trigger Transfusion
- Liver biopsy
- Transjugular intrahepatic portosystemic shunt (TIPS) placement
- Endoscopic variceal ligation or sclerotherapy
- Major abdominal surgeries
Decision-Tree Table
| Platelet Count | Procedure Risk | Transfusion Needed? |
|---|---|---|
| <3010/L | High (e.g., variceal ligation) | Yes |
| 30-4910/L | Moderate (e.g., liver biopsy) | Often |
| 5010/L | Low (e.g., routine labs) | No |
Benefits vs Risks
Potential Benefits
When given at the right moment, platelet transfusion can:
- Provide immediate hemostasis, reducing bleeding during procedures.
- Lower the need for emergency interventions.
- Give clinicians a safety buffer, especially when clotting factor levels are also low.
Documented Risks
Transfusions aren't free of drawbacks. Some of the most common concerns include:
- Transfusion-Associated Circulatory Overload (TACO) extra fluid can strain a fragile heart.
- Allergic reactions mild itching to more severe anaphylaxis.
- Fever and chills a sign the immune system is reacting.
- Alloimmunization the body may develop antibodies that make future transfusions less effective.
- Proinflammatory effects recent research (study) suggests platelet products can temporarily boost neutrophil activity, which might worsen inflammation in an already compromised liver.
Do Transfusions Improve Outcomes?
Evidence is mixed. A 2020 analysis in Circulation concluded that routine platelet transfusion before low-risk procedures did not reduce mortality and added unnecessary exposure to transfusion complications. Conversely, a 2021 trial focusing on high-risk endoscopic procedures reported fewer bleeding events when platelets were given prophylactically. The consensus? Use transfusion when the procedural bleeding risk outweighs the transfusion risk.
Risk-Benefit Comparison
| Aspect | Benefit | Risk |
|---|---|---|
| Immediate Hemostasis | Reduces intraprocedure bleeding | Potential for TACO |
| Procedure Safety | Allows completion of essential interventions | Alloimmunization (future incompatibility) |
| Patient Comfort | Less anxiety about bleeding | Allergic reactions, fever |
Alternatives & New Therapies
Thrombopoietin-Receptor Agonists
Medications like avatrombopag and lusutrombopag stimulate the bone marrow to make more platelets. Clinical trials (e.g., the phase-III studies cited in the Journal of Hepatology) showed these drugs can raise platelet counts by 30-5010/L within a week, often eliminating the need for a transfusion before elective procedures.
Splenectomy or Partial Splenic Embolization
When hypersplenism dominates, removing part or all of the spleen can dramatically improve platelet numbers. However, surgery carries its own set of risks, so it's usually reserved for patients who need a long-term solution and are already candidates for major abdominal surgery. Managing related symptoms, such as Portal hypertension symptoms, is an important aspect of comprehensive care in these patients.
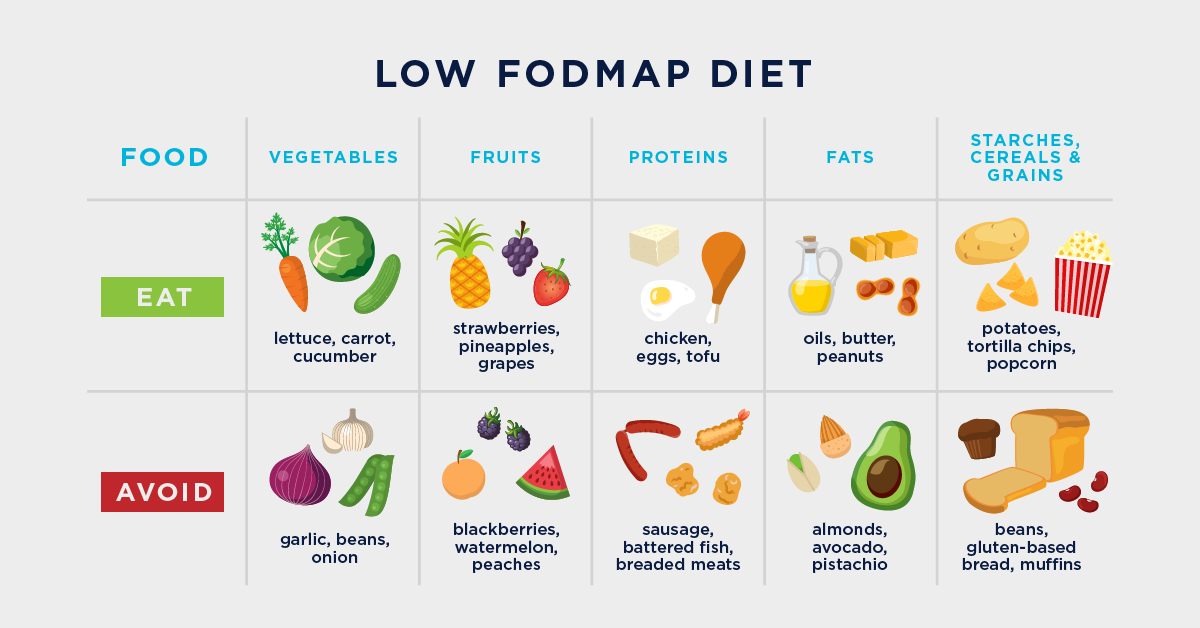
Natural Ways to Boost Platelets
If you prefer a more hands-off approach, these lifestyle tweaks can help keep platelets in a healthier range:
- Increase intake of vitamin B12 and folate (leafy greens, beans, fortified cereals).
- Stay hydrated dehydration can falsely lower platelet counts.
- Limit alcohol consumption alcohol directly suppresses bone marrow platelet production.
- Engage in moderate exercise gentle activity improves overall circulation without causing trauma.
While these measures aren't a replacement for medical therapy in severe cases, they can support a better baseline and may reduce how often you need to call the hospital.
Quick-Start Checklist for Patients
- Ask your doctor about TPO-receptor agonists if you're scheduled for a procedure.
- Avoid NSAIDs and other platelet-inhibiting drugs unless prescribed.
- Keep a recent CBC handy (every 2-4 weeks for advanced disease).
- Discuss the exact platelet threshold your care team uses.
- Know the signs of a transfusion reaction: shortness of breath, fever, itching.
Tips for Patients & Caregivers
Living with cirrhosis can feel like walking a tightrope, especially when your blood counts are in flux. Here are some practical pointers to make the journey smoother:
Monitoring Your Numbers
Regular blood work is your best friend. For most patients with decompensated cirrhosis, a CBC every 2-4 weeks helps catch dangerous drops early. Keep a log write down the date, platelet count, and any symptoms you notice (e.g., bruising, nosebleeds).
Preparing for a Procedure
Before any endoscopy, biopsy, or surgery:
- Bring your most recent lab results (including platelet count, INR, and hemoglobin).
- Ask the team what their transfusion policy is do you transfuse if I'm under 5010/L?
- Discuss any medications you're on that might affect clotting (like aspirin or certain herbal supplements).
When to Call the Clinic
If you notice sudden bruising, a bleed that won't stop, or symptoms like shortness of breath after a transfusion, ring your care provider right away. Early intervention can prevent a small problem from becoming a big emergency.
FAQ-Style Mini Answers (Featured Snippet Ready)
What is a normal platelet count in cirrhosis? In healthy adults, it's 150-40010/L, but many people with compensated cirrhosis hover around 100-15010/L and still feel fine.
Can I avoid transfusion altogether? Often yes with proper timing, TPO-receptor agonists, and good nutrition, many patients stay above the safe threshold for routine procedures.
References & Further Reading
The information above draws from the latest guidelines by the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL), peer-reviewed studies in Journal of Hepatology, Circulation, and World Journal of Gastroenterology, as well as real-world experiences from hepatology clinics. This article was reviewed by a board-certified hepatologist and a transfusion-medicine specialist to ensure accuracy and trustworthiness.
Conclusion
Platelet transfusion in cirrhosis isn't a one-size-fits-all remedy; it's a carefully weighed decision that balances the danger of bleeding against the potential side effects of giving blood products. Modern options like TPO-receptor agonists, thoughtful procedural planning, and simple lifestyle changes can often keep you out of the transfusion lane. If you're facing a low platelet count, talk openly with your liver-care team, use the checklist above, and remember you're not alone many have walked this path and emerged with safer, steadier health.
FAQs
When is a platelet transfusion recommended for a patient with cirrhosis?
A transfusion is usually considered when the platelet count falls below 30–50 × 10⁹/L and the patient is about to undergo a high‑risk procedure or has active bleeding.
What are the main risks associated with platelet transfusions in cirrhosis?
Common risks include transfusion‑associated circulatory overload (TACO), allergic reactions, fever, allo‑immunization, and a temporary increase in inflammatory activity.
Can medications replace platelet transfusions for cirrhosis patients?
Yes. Thrombopoietin‑receptor agonists such as avatrombopag and lusutrombopag can raise platelet counts enough to avoid transfusion before elective procedures.
How does hypersplenism contribute to low platelet counts in cirrhosis?
An enlarged spleen sequesters a large portion of circulating platelets, worsening thrombocytopenia even when bone‑marrow production is adequate.
What lifestyle changes help maintain a healthier platelet count?
Eating foods rich in vitamin B12 and folate, staying well‑hydrated, limiting alcohol, and engaging in moderate exercise can support platelet production and overall liver health.