Quick Answers First
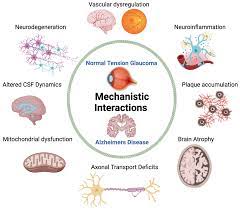
What are the main causes of normal tension glaucoma?
In a nutshell, normal tension glaucoma (NTG) usually stems from vascular insufficiencybasically, the optic nerve isnt getting enough blood flowplus a few other culprits like migrainerelated vasospasms, nighttime bloodpressure dips, and structural quirks of the eye itself. These factors can damage the optic nerve even when intraocular pressure (IOP) stays normal.
Will I go blind from normaltension glaucoma?
The short answer: it can lead to significant vision loss if left untreated, but early detection and targeted treatment dramatically lower that risk. Think of it like catching a leak early before it floods your house.
Is normal tension glaucoma hereditary?
There is a genetic component, but its not the whole story. Family history does raise risk, yet most cases are driven by vascular and systemic factors rather than pure inheritance.
Core Root Causes
1. Vascular Insufficiency & Optic Nerve Perfusion
When the tiny blood vessels that feed the optic nerve dont deliver enough oxygen, the nerve fibers start to wither. This lowflow theory is supported by several studies, including a that showed reduced ocular blood flow in NTG patients compared to those with highpressure glaucoma.
Key points in this category:
- Chronic lowbloodflow: Longterm subtle reductions in circulation can slowly chip away at nerve cells.
- Nocturnal systemic hypotension: Blood pressure that drops too low at night can starve the optic nerve of oxygen while youre sleeping.
- Raynauds phenomenon: If your fingers turn white in the cold, the same vasospasm could be happening in your eye.
2. Migraine & Vascular Spasms
People who suffer from migraines often experience vascular spasmsbrief, intense squeezes of blood vessels. When this happens in the eyes microcirculation, it can act like a ministroke for the optic nerve. A recent review from the Mayo Clinic notes that migraine sufferers have a 23fold higher chance of developing NTG.
Realworld example: Mike, a 58yearold accountant, began noticing peripheral vision loss after years of chronic migraines. Once his neurologist introduced a migraine prophylactic, his visual field stabilized, illustrating how treating the vascular component can help.
3. BloodPressure Extremes
Both ends of the pressure spectrum are troublemakers. Overtreated hypertension can push your systolic numbers so low that the eyes blood supply suffers, while deep nighttime dips in blood pressure (often seen in people with sleep apnea) can cause the same problem.
| Condition | Impact on Optic Nerve | Typical Management |
|---|---|---|
| Overtreated hypertension | Reduced ocular perfusion pressure | Adjust meds with primarycare doctor |
| Nocturnal hypotension | Nighttime optic nerve ischemia | 24hr BP monitoring, medication timing |
| Sleep apnea | Intermittent hypoxia, vascular stress | CPAP therapy, weight management |
4. Structural/Anatomical Vulnerabilities
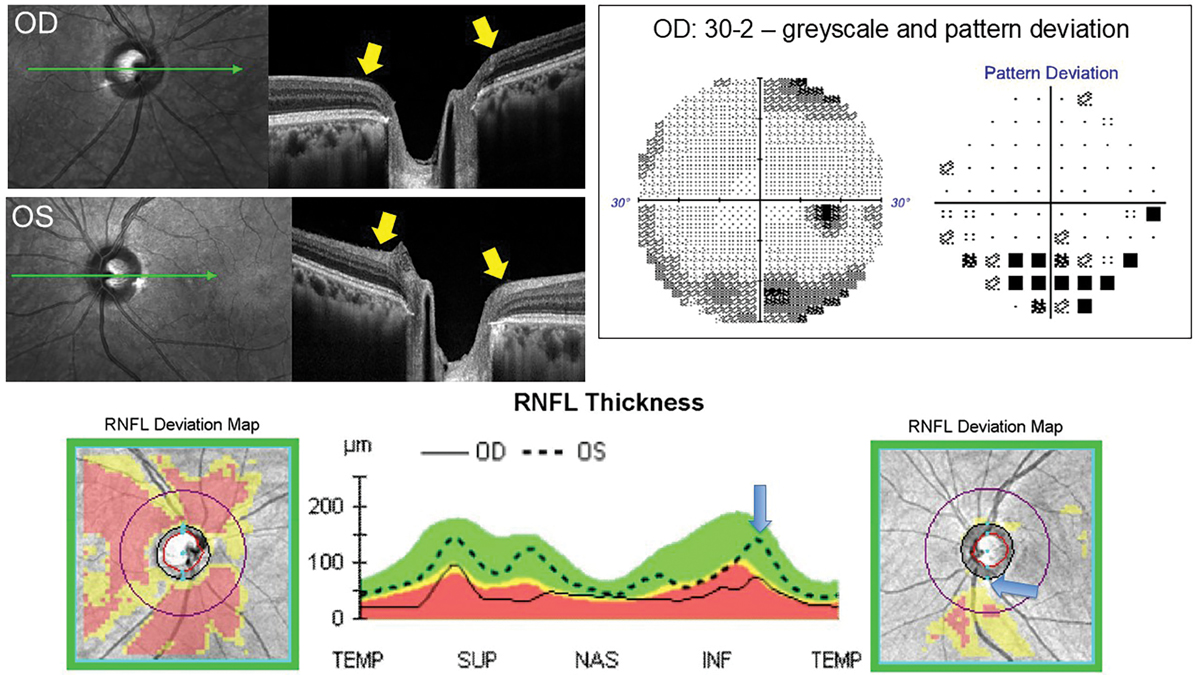
Some eyes are simply built differently. A thin lamina cribrosa (the window through which nerve fibers exit the eye) can make those fibers more vulnerable to even modest drops in blood flow. Optical coherence tomography (OCT) often reveals a characteristic cupping pattern in NTG that hints at this structural susceptibility.
5. Other Contributing Factors
- Autoimmune / inflammatory conditions: Diseases like lupus can cause subtle inflammation around the optic nerve.
- Sleep apnea: The repeated oxygen dips stress the vascular system.
- Lifestyle choices: Smoking, excessive caffeine, and poor sleep can all tighten up blood vessels.
Progression Speed Guide
Typical progression timeline
On average, NTG patients lose about 0.51.0 decibels (dB) of visualfield sensitivity per year, but the rate varies widely. Those with pronounced vascular issues often progress faster, while wellcontrolled patients may see a nearstable field for years.
Factors that accelerate progression
- Uncontrolled nighttime hypotension
- Poor adherence to eyedrop regimen
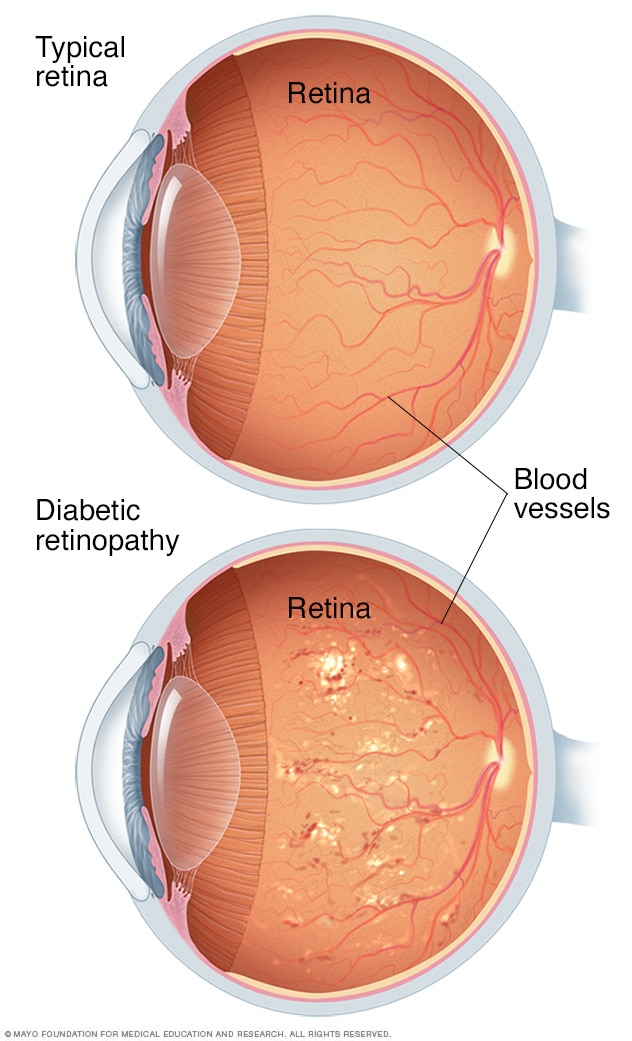
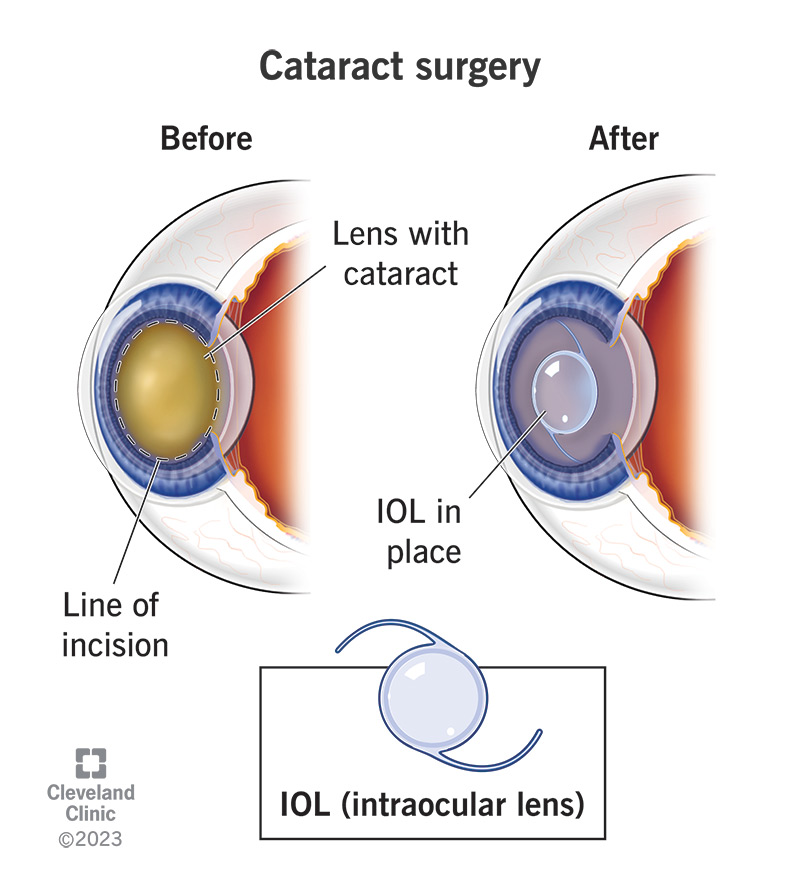
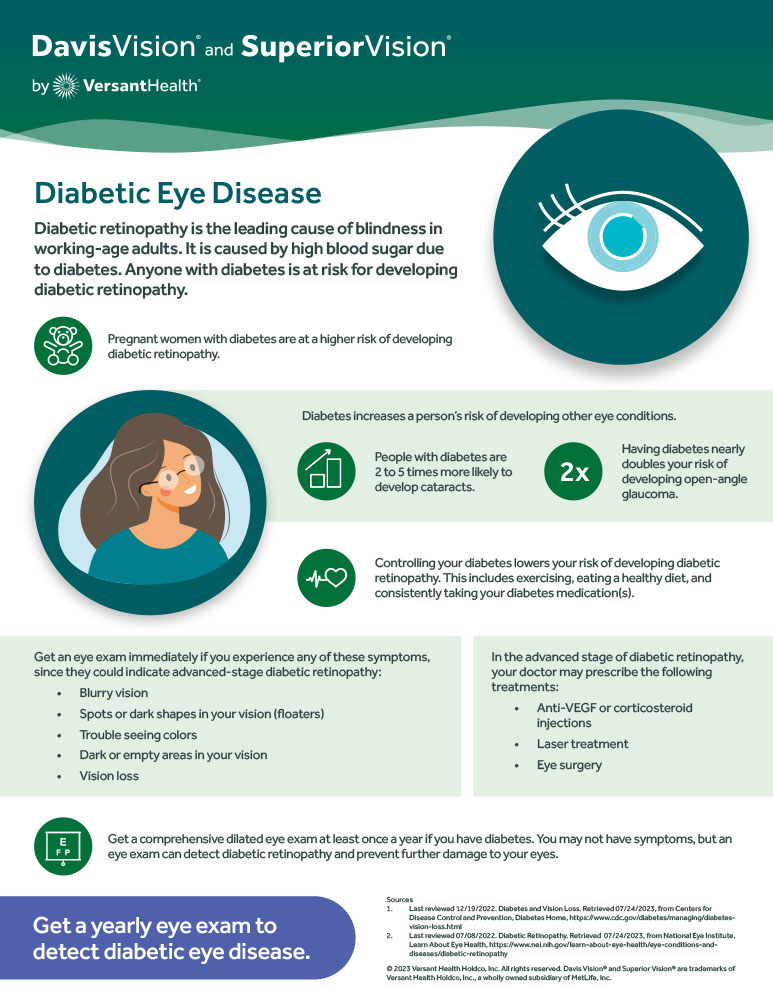
- Concurrent eye diseases (e.g., cataract, diabetic retinopathy)
- Continued smoking or heavy caffeine intake
When to seek urgent care
If you notice sudden loss of peripheral vision, new shadow in your sight, or a sharp dip in visualfield test results, call your eye doctor right away. These redflags can signal rapid progression that needs immediate intervention.
How It's Diagnosed
Key clinical tests
Diagnosing NTG is a bit like detective work because the pressure numbers look normal. Doctors rely on:
- Intraocular pressure (IOP) measurement: Shows that pressure isnt the primary villain.
- Optical coherence tomography (OCT): Highlights thinning of the retinal nervefiber layer, a hallmark of NTG.
- Visualfield testing (Humphrey): Maps out the blind spots that develop over time.
According to the American Academy of Ophthalmology, combining these tests improves diagnostic accuracy dramatically.
Differential diagnosis
Doctors must separate NTG from primary openangle glaucoma (where IOP is high) and from nonglaucomatous optic neuropathies like ischemic optic neuropathy. A sidebyside comparison helps:
| Feature | Normal Tension Glaucoma | OpenAngle Glaucoma | Ischemic Optic Neuropathy |
|---|---|---|---|
| IOP | Normal (21mmHg) | Elevated | Variable |
| OCT RNFL | Selective thinning, often inferior | Diffuse thinning | Sectoral loss |
| Visual Field | Peripheral loss, arcuate defects | Progressive, often centralperipheral | Sudden, altitudinal |
Role of systemic workup
Because bloodflow issues are frontandcenter, many specialists order a 24hour bloodpressure monitor and sometimes a Doppler ultrasound of the carotid arteries. Collaboration between your ophthalmologist, primarycare physician, and possibly a cardiologist ensures that the vascular side of the disease gets the attention it deserves.
Treatment & Management
Lowering IOP even when its normal
It might sound odd, but dropping IOP a few points can still protect the optic nerve by improving perfusion pressure. Firstline options include prostaglandin analogues (like latanoprost), which are oncedaily drops that most patients tolerate well. For those who need a boost, laser trabeculoplasty or minimally invasive glaucoma surgery (MIGS) can be considered.
Addressing vascular contributors
Think of NTG as a twofront battle: you lower IOP and you fix the bloodflow problem.
- Bloodpressure optimization: Adjust antihypertensive meds to avoid deep nighttime dips. Some doctors shift the timing of medication to the morning.
- Migraine prophylaxis: Meds such as betablockers or topiramate may reduce vasospasms.
- Lifestyle tweaks: Regular aerobic exercise improves overall circulation; moderate caffeine (no more than 2 cups of coffee a day) is usually safe.
Monitoring and followup
Consistency is key. Most clinicians schedule OCT and visualfield tests every 612 months for stable patients, tightening the interval if the disease shows signs of progression.
Future therapies & research
Scientists are exploring neuroprotective agentsdrugs that directly shield retinal ganglion cells. One promising candidate, brimonidine, showed modest benefit in a 2023 clinical trial (). Genetherapy trials are also on the horizon, aiming to correct underlying vascular genes.
Balancing Benefits Risks
Why understanding causes matters
When you know whether a migraine or low nighttime blood pressure is the main driver, you can target that factor directly. Its like fixing the leak at its source rather than constantly mopping the floor.
Potential sideeffects of treatments
Eye drops can cause mild irritation, redness, or occasional eyelash changes. Surgical options carry standard risksinfection, shortterm glarebut theyre rare when performed by an experienced surgeon.
Shared decisionmaking with your eyecare team
Ask your doctor questions like:
- How does my bloodpressure profile affect my glaucoma?
- Would a migraine medication help my eye health?
- What monitoring schedule do you recommend for me?
Being an active participant ensures the plan fits your lifestyle and comfort level.
Final Takeaway
Normal tension glaucoma is a stealthy condition where the enemy isnt high pressure but a whisper of insufficient blood flow, migraines, nighttime hypotension, and even the way your eye is built. The good news? Early detection, a personalized mix of IOPlowering drops, vascularfocused lifestyle tweaks, and regular monitoring can keep the disease in check and preserve your vision for years to come.
If you suspect any changes in your peripheral vision or have a family history of glaucoma, schedule an eye exam today. And why not download a free NTG RiskTracker checklist to stay on top of your health? Your eyes deserve the same care you give the rest of your bodylets keep them sharp together.
FAQs
What primary factor leads to normal tension glaucoma?
The most widely accepted cause is vascular insufficiency—reduced blood flow to the optic nerve that starves nerve fibers of oxygen, even when intra‑ocular pressure is within the normal range.
How do migraines contribute to the development of NTG?
Migraine attacks involve brief vasospasms of small blood vessels. When these spasms affect the eye’s micro‑circulation, they can create miniature strokes that damage the optic nerve, raising the risk of NTG.
Can low nighttime blood pressure trigger or worsen NTG?
Yes. Nocturnal hypotension lowers ocular perfusion pressure while you sleep, leading to intermittent ischemia of the optic nerve and accelerating visual‑field loss.
Is a thin lamina cribrosa a cause of NTG or just a risk factor?
A thin or structurally weak lamina cribrosa makes optic‑nerve fibers more vulnerable to even modest reductions in blood flow, acting as a predisposing risk factor rather than a direct cause.
What lifestyle changes help reduce the risk of NTG progression?
Regular aerobic exercise, moderate caffeine intake, quitting smoking, managing hypertension without excessive nighttime dips, and treating sleep apnea can all improve ocular blood flow and slow disease progression.