Quick Answers Overview
What does final stage really mean? Its the point when the heart can no longer pump enough blood to meet the bodys needs, even with maximum medications and devices. Symptoms are severe, daily activities become impossible, and life expectancy usually shrinks to weekstomonths.
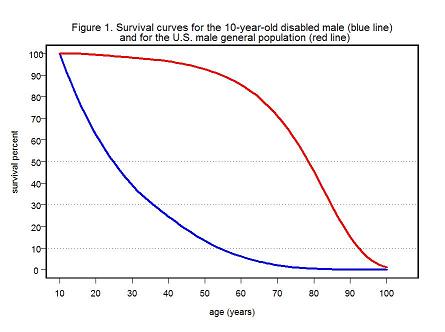
How long might an 85yearold expect to live? On average, an elderly patient with endstage CHF survives312months, but the range is wide. Other illnesses, functional status, and whether palliative care is involved can push that number a little higher or lower.
Clinical Picture Overview
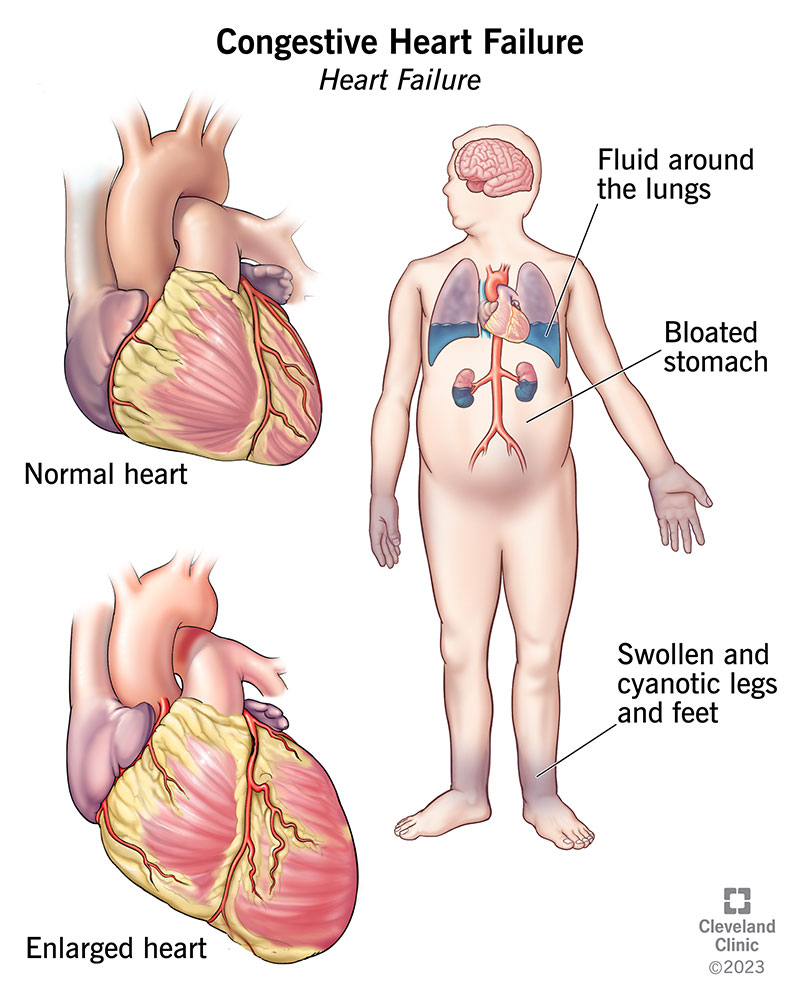
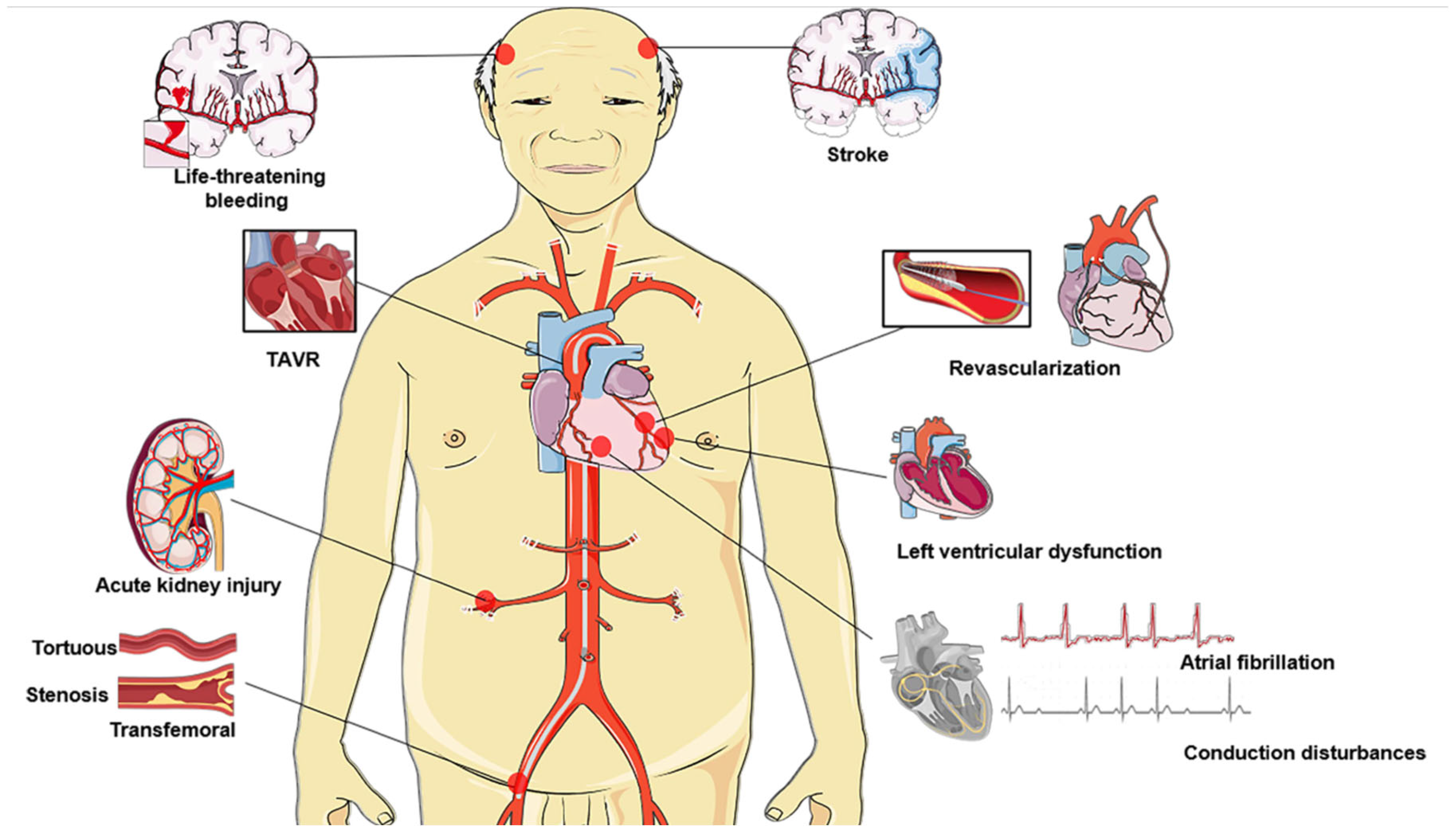
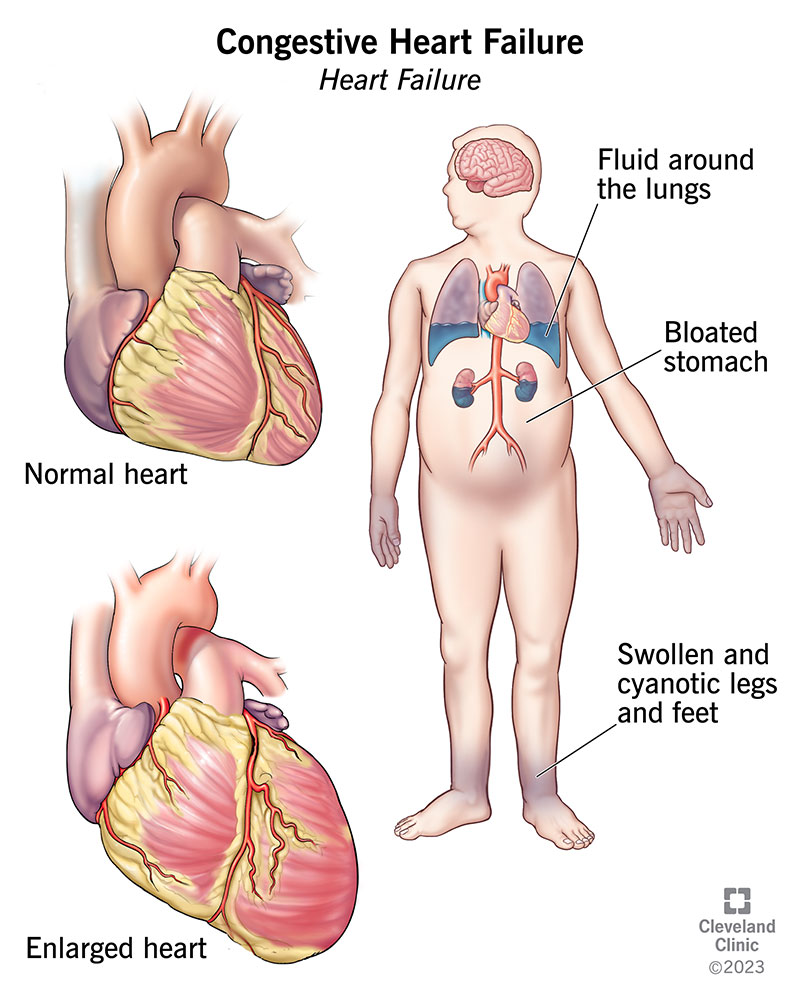
What defines the final stage (StageD / Stage5) CHF?
StageD, sometimes called Stage5, is the endstage classification in the guidelines. Its diagnosed when a patient has:
- Leftventricular ejection fraction (LVEF) usually below20%.
- Refractory symptoms despite optimal medical therapy, diuretics, and devicebased treatments.
- Frequent hospitalizations for fluid overload or arrhythmias.
- Reliance on specialized heartfailure clinics for daily management.
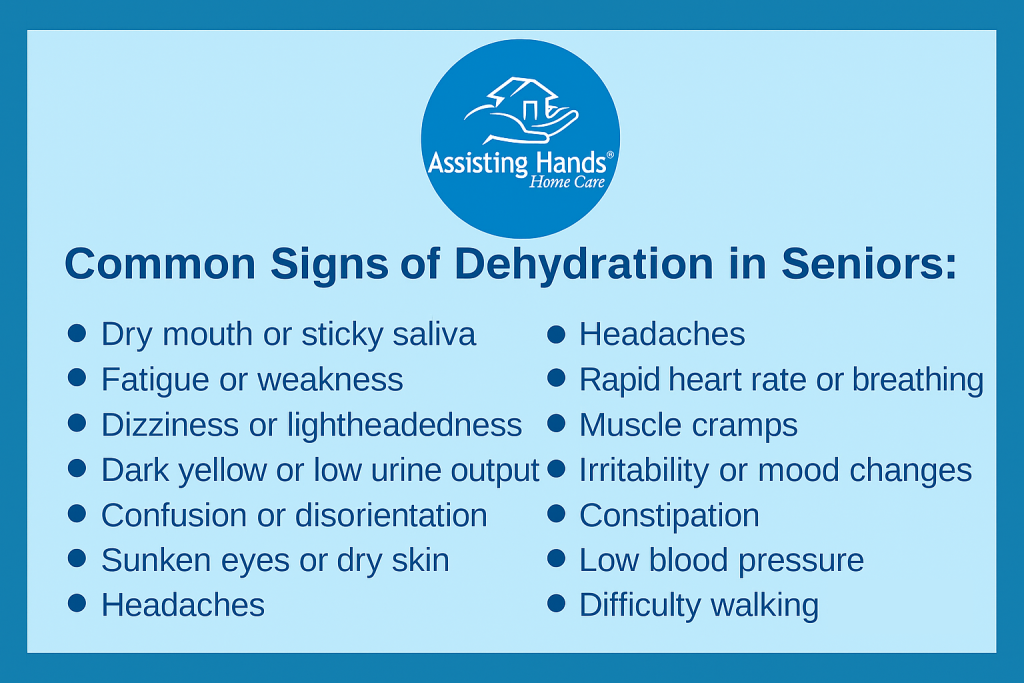
Common signs and symptoms in the elderly
When the heart is on its last legs, the body sends loud, unmistakable signals. Older adults often notice:
| Symptom | What to Watch For | When to Call Help |
|---|---|---|
| Breathlessness at rest | Sudden inability to finish a sentence without gasping | Immediately could signal acute pulmonary edema |
| Swollen ankles/abdomen | Rapid weight gain of2kg in 24hours | Contact cardiology if diuretics no longer work |
| Extreme fatigue | Inability to sit up or hold a cup of tea | Within a day if paired with confusion |
| Confusion or disorientation | Repetitive questions, forgotten names | Urgent may indicate low perfusion to the brain |
How long does the final stage usually last?
Studies from the show a median survival of roughly5months after entering StageD, but many patients live as little as a few weeks or as long as a year, depending on coexisting conditions like kidney disease, COPD, or frailty.
Is death from CHF sudden or gradual?
Most deaths in endstage heart failure are gradual the body slowly gives up as fluid backs up, organs receive less oxygen, and infections take hold. A sudden cardiac arrest can still happen, especially if dangerous arrhythmias develop, but thats the exception rather than the rule.
Impending Death Indicators
Key warning signs of imminent decline
When the clock is truly winding down, families often notice a shift:
- Marked decrease in alertness the person spends most of the day sleeping.
- Restlessness or terminal agitation, sometimes described as pulling blankets off.
- Reduced oral intake fluids and food may disappear almost overnight.
- Changes in breathing pattern long pauses followed by shallow breaths (CheyneStokes).
These signs dont mean the end is minutes away, but they do suggest that the next few weeks are likely the most critical phase.
Differentiating irreversible decline from treatable flareups
Its easy to mistake a treatable fluid overload for the final stretch. The difference often lies in response to therapy:
- If a higher dose of diuretics and a shortterm IV line rapidly improve breathing, youre probably dealing with an acute exacerbation.
- If symptoms persist despite aggressive diuresis, oxygen, and medication adjustments, the decline is more likely irreversible.
Red Flags vs. Manageable Symptoms
| Red Flag (Impending Death) | Manageable Symptom (Treatable) |
|---|---|
| Profound lethargy, unresponsive to stimuli | Shortness of breath that eases with diuretics |
| Loss of appetite for >48hours | Morning swelling that reduces by evening |
| Irregular, shallow breathing cycles | Chest discomfort that responds to nitrates |
Life Expectancy Guide
Statistical outlook for an 85yearold
Data from indicate that an 85yearold in StageD has a median survival of about8months. Factors that can shorten this include:
- Severe kidney failure (eGFR<30ml/min)
- Advanced dementia or severe cognitive decline
- Repeated hospital admissions for pulmonary edema
Conversely, patients who maintain a degree of mobility, have good nutritional status, and receive early palliative involvement may exceed a year.
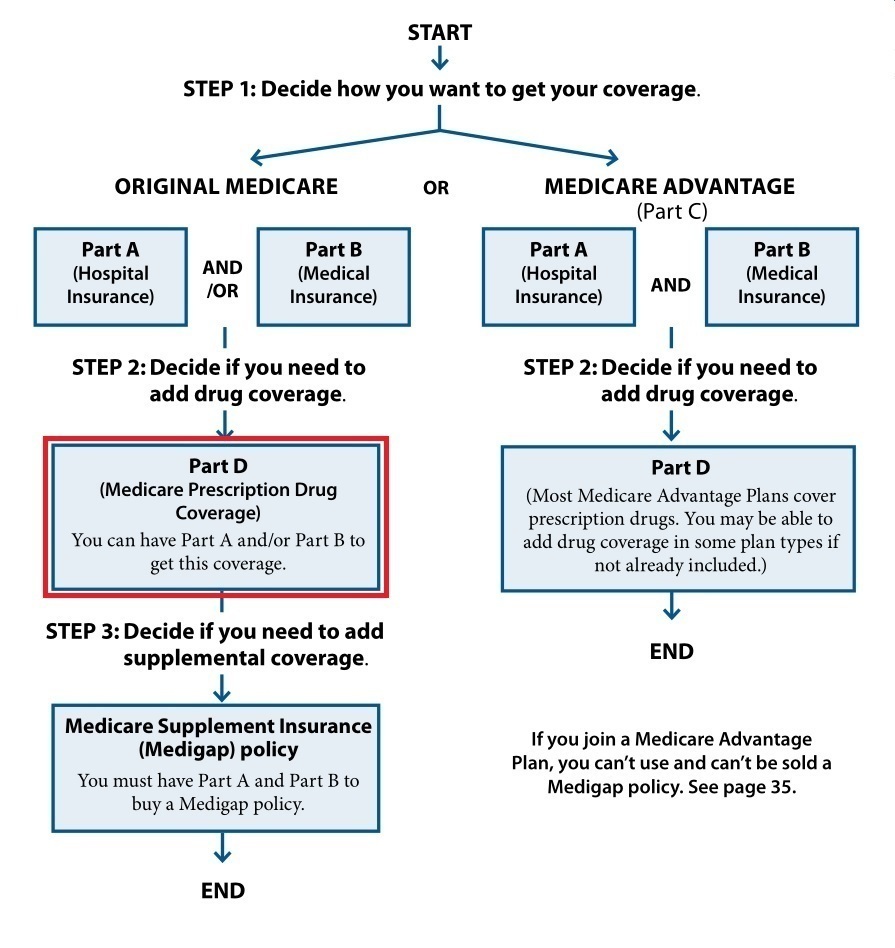
Advanced care planning essentials
Talking about the end feels uncomfortable, yet its one of the most caring things you can do. Key documents to consider:
- DNR (DoNotResuscitate) order clarifies wishes about CPR.
- POLST (Physician Orders for LifeSustaining Treatment) translates broader goals into concrete medical orders.
- Advance directive outlines preferences for ventilation, feeding tubes, and hospice enrollment.
Invite your loved ones primary cardiologist, a palliativecare physician, and a trusted family member to the conversation. Listening first, then sharing information, creates a collaborative plan that respects the patients values.
When to consider hospice or palliative sedation
If the goal shifts from extending life at any cost to maximizing comfort, hospice becomes a natural next step. Hospice teams bring expertise in:
- Medication titration for breathlessness (lowdose morphine, benzos).
- Emotional and spiritual support for the whole family.
- Homebased nursing that can manage IV diuretics or wound care.
Palliative sedationusing medications to relieve intractable sufferingmay be discussed only when symptoms cannot be controlled by any other means. It is always a shared decision, never a unilateral one.
Comfort Symptom Management
Relieving breathlessness
Dyspnea is the hallmark of endstage CHF. Practical, lowtech tricks can make a huge difference:
- Positioning: sitting upright with a pillow behind the back, or using a tripod position with arms on a table.
- Fans: a gentle breeze across the face reduces the sensation of breathlessness.
- Lowdose opioids (e.g., morphine 25mg PO q4h) have solid evidence for easing dyspnea without causing respiratory depression when titrated carefully.
Controlling fluid overload and edema
Even in the final phase, gentle diuresis can improve comfort:
- Loop diuretics (furosemide) IV or PO, adjusted to kidney function.
- Thiazide addon (e.g., metolazone) for diuretic resistance.
- Lowsodium diet (under2g per day) and fluid restriction (11.5L/day) if tolerated.
Compression stockings may be soothing for leg swelling, but ensure they are not too tightcirculation is already compromised.
Managing pain, anxiety, depression
Physical discomfort often intertwines with emotional distress. A multimodal approach works best:
- Nonpharmacologic: gentle music, guided imagery, and short walks (if possible).
- Pharmacologic: lowdose morphine for pain and breathlessness; shortacting benzodiazepines (lorazepam 0.5mg q6h PRN) for anxiety or terminal restlessness.
- Antidepressants (e.g., sertraline) may be started early; they take weeks to work, so theyre more useful for chronic sadness rather than acute crisis.
Sample medication chart for the elderly
| Medication | Typical Dose (Elderly) | Purpose | Notes |
|---|---|---|---|
| Furosemide | 2040mg PO daily (adjust up to 80mg) | Diuresis | Monitor electrolytes and kidney function. |
| Morphine | 25mg PO q4h PRN dyspnea | Breathlessness & pain | Start low; watch for constipation. |
| Lorazepam | 0.5mg PO q6h PRN anxiety | Anxiety/terminal restlessness | Avoid longterm use due to fall risk. |
| Sertraline | 25mg PO daily | Depression | May take 24 weeks for effect. |
Nutrition and hydration tips
Appetite often wanes, but dehydration can worsen kidney function and increase delirium risk. Small, frequent mealsthink half a banana, a spoonful of yogurt, or a sip of clear brothare easier to tolerate than large plates. If oral intake is insufficient, discuss comfortfocused hydration with the hospice team; the goal is symptom relief, not aggressive fluid replacement.
Real World Experiences
Case study: Mr. J., 86, StageD CHF
Mr. J. lived alone in a small town. After two hospitalizations for pulmonary edema, his cardiologist labeled him StageD. He chose hospice after a family meeting, and the team introduced lowdose morphine for dyspnea and a gentle diuretic regimen. Within weeks, his breathlessness eased, he slept through the night, and his family reported a sense of peace that hadnt existed during his last hospital stay. He passed quietly in his own chair, holding his daughters handexactly the dignified ending hed hoped for.
Family caregiver stories
Emily, a granddaughter, shared that the nighttime panic she felt when her mothers breathing became irregular was overwhelming. A simple fan, a soft pillow to prop the head up, and a quick call to the hospice nurse turned those terrifying moments into manageable ones. It wasnt the death that scared me, she wrote, it was the feeling of not knowing what to do. Knowing there was a plan helped my heart more than any medicine could.
Expert insights (interview suggestions)
When you flesh out the full article, consider quoting:
- Dr. Laura Martinez, MD, boardcertified cardiologist, who can explain why ejection fraction <20% is a red flag.
- Grace Liu, RN, hospice clinical specialist, who can detail how a comfortfirst medication protocol is built.
- Statistics from the that compare survival curves across age groups.
These voices add authority and make the information feel less like a textbook and more like a conversation with trusted friends.
Additional Resources & References
For deeper dives, you might explore the following reputable sources:
Conclusion
Walking through the final stages of congestive heart failure in the elderly is never easy, but understanding the signs, the likely timeline, and the caring options available can turn anxiety into actionable hope. Whether youre a family member, a caregiver, or the patient yourself, remember that the goal shifts from curing to comforting. Talk openly with doctors, consider hospice early, and lean on the expertise of palliative teamstheyre there to make the last chapter as gentle as possible.
What experiences have you had with endstage heart failure? Share your story in the comments, or reach out if you have questions. Together, we can navigate this tough journey with compassion and clarity.
FAQs
What is the typical life expectancy for an 85‑year‑old in the final stage of CHF?
Most studies show a median survival of 5‑8 months after entering Stage D, but the range can be from a few weeks to over a year depending on comorbidities and functional status.
How can families tell the difference between a treatable fluid overload and irreversible decline?
If high‑dose diuretics, short‑term IV therapy, or oxygen quickly improve breathing, it’s likely a reversible exacerbation. Persistent symptoms despite aggressive treatment suggest an irreversible end‑stage decline.
When is the right time to consider hospice for an elderly patient with end‑stage CHF?
When the focus shifts from extending life to maximizing comfort—typically when hospital readmissions become frequent, breathlessness remains despite maximal therapy, or the patient expresses a desire for less invasive care.
Are low‑dose opioids safe for relieving dyspnea in frail seniors?
Yes. Morphine 2‑5 mg orally every 4 hours (adjusted for kidney function) is effective for breathlessness and does not cause respiratory depression when started low and titrated carefully.
What practical tips help caregivers manage daily comfort at home?
Use upright or tripod positioning, a bedside fan for airflow, small frequent meals, regular weight checks, and keep a “quick‑call” list of hospice nurses and the cardiology team for any sudden change.