What is COVID Heart Failure
In plain language, COVID heart failure is when the coronavirus triggers inflammation, clotting, or direct injury that weakens the hearts pumping power. Its not a completely new diseaseits the same heartfailure syndrome youd see from other causes, but the virus can accelerate or ignite the process.
How does SARSCoV2 damage the heart?
Scientists have identified three main pathways:
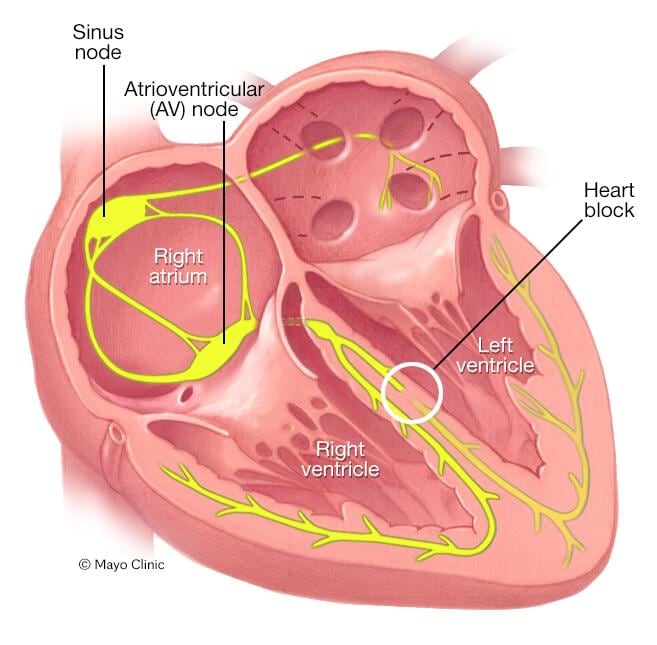
- Inflammation & cytokine storm: The bodys fierce immune response can inflame the heart muscle, a condition known as myocarditis.
- Direct viral infiltration: The virus can actually invade heart cells, disrupting their function. , this direct damage is more common than we once thought.
- Bloodclot formation: COVID increases clot risk, which can block coronary arteries and lead to heartmuscle death.
Is it the same as preexisting heart failure?
While the end resultreduced cardiac outputis similar, COVIDrelated cases often appear suddenly, even in people with no prior cardiac history. The triggers, timing, and shortterm prognosis can differ, so doctors treat it with a blend of standard heartfailure therapy and COVIDspecific care.
How Common Are Heart Issues
Understanding the odds helps keep anxiety in check. Recent research paints a clear picture.
Incidence after infection
Largescale analyses from the NIH and other health agencies show that people whove recovered from COVID are about twice as likely to develop a heart problem within three years compared with those who never contracted the virus.
| Severity of COVID | HeartFailure Risk (per 1,000) |
|---|---|
| Mild (no hospitalization) | 57 |
| Moderate (hospital stay) | 1215 |
| Severe (ICU/ventilator) | 2835 |
These numbers come from a 2024 UNMC cohort that followed 5,000 patients across five continents. , the risk climbs further if you already have hypertension, diabetes, or a prior heart condition.
Who is most at risk?
Age over 60, male gender, and preexisting cardiovascular disease dramatically raise the odds. If youre wondering is COVID dangerous for heart patients? the answer is a cautious yesbut the danger is far lower if youre fully vaccinated.
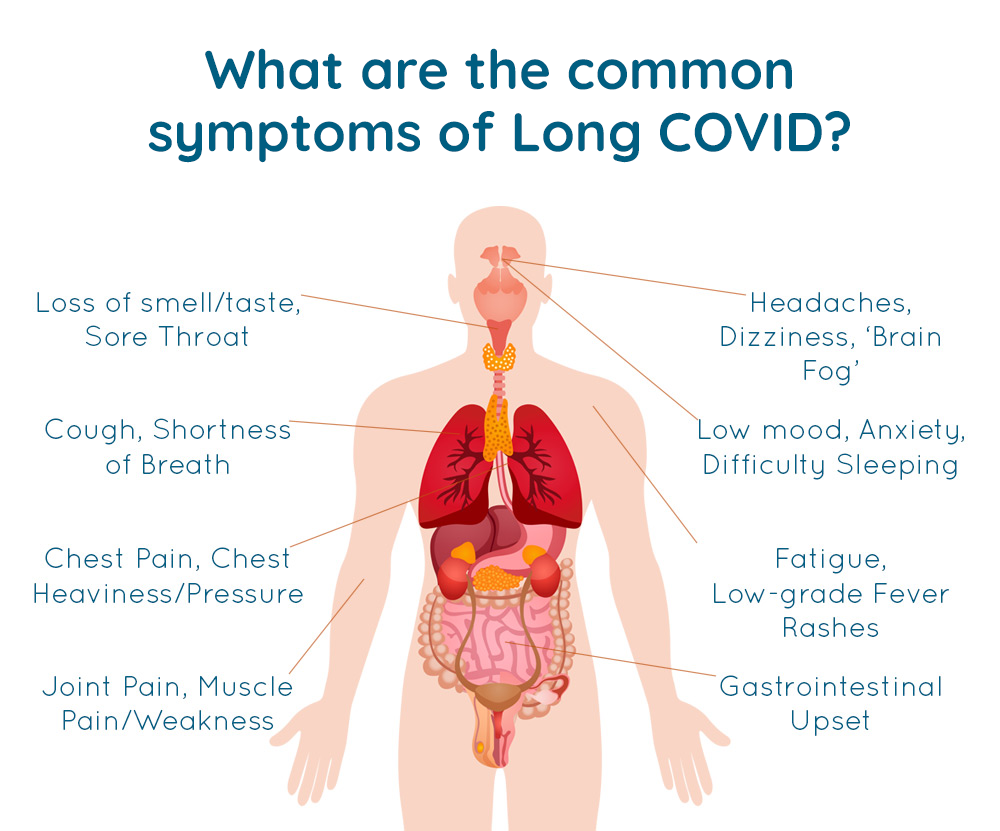
Warning Signs & Symptoms
Spotting trouble early can be lifesaving. Below are the red flags that most people overlook.
Early red flags you cant ignore
- Persistent chest discomfort or pressure
- Shortness of breath that worsens with light activity
- Unexplained fatigue lasting weeks after the infection clears
- Swelling in ankles or feet if swelling persists it can be a sign of heart failure edema and deserves prompt evaluation.
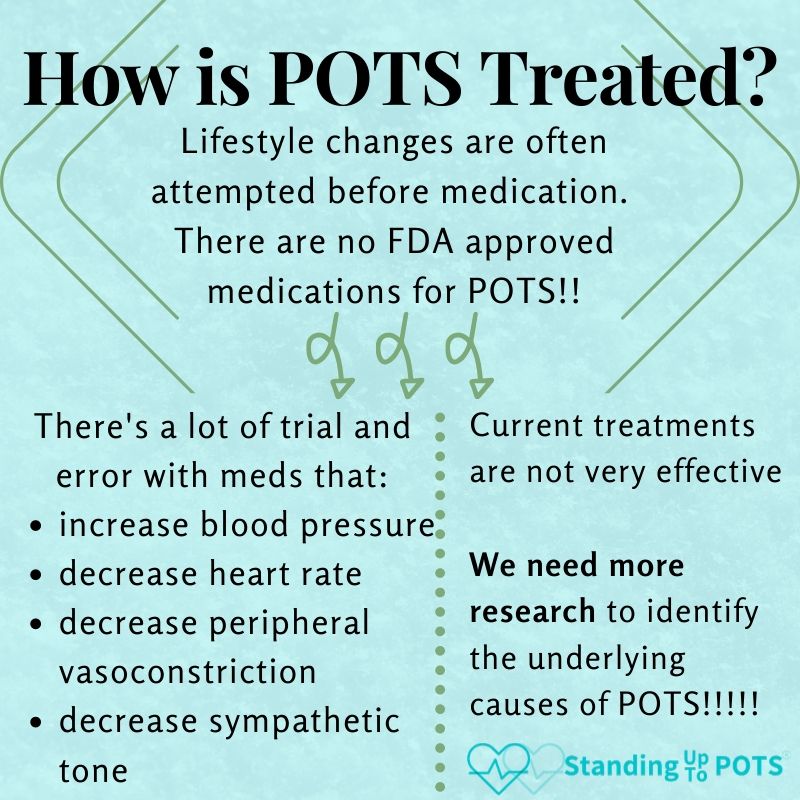
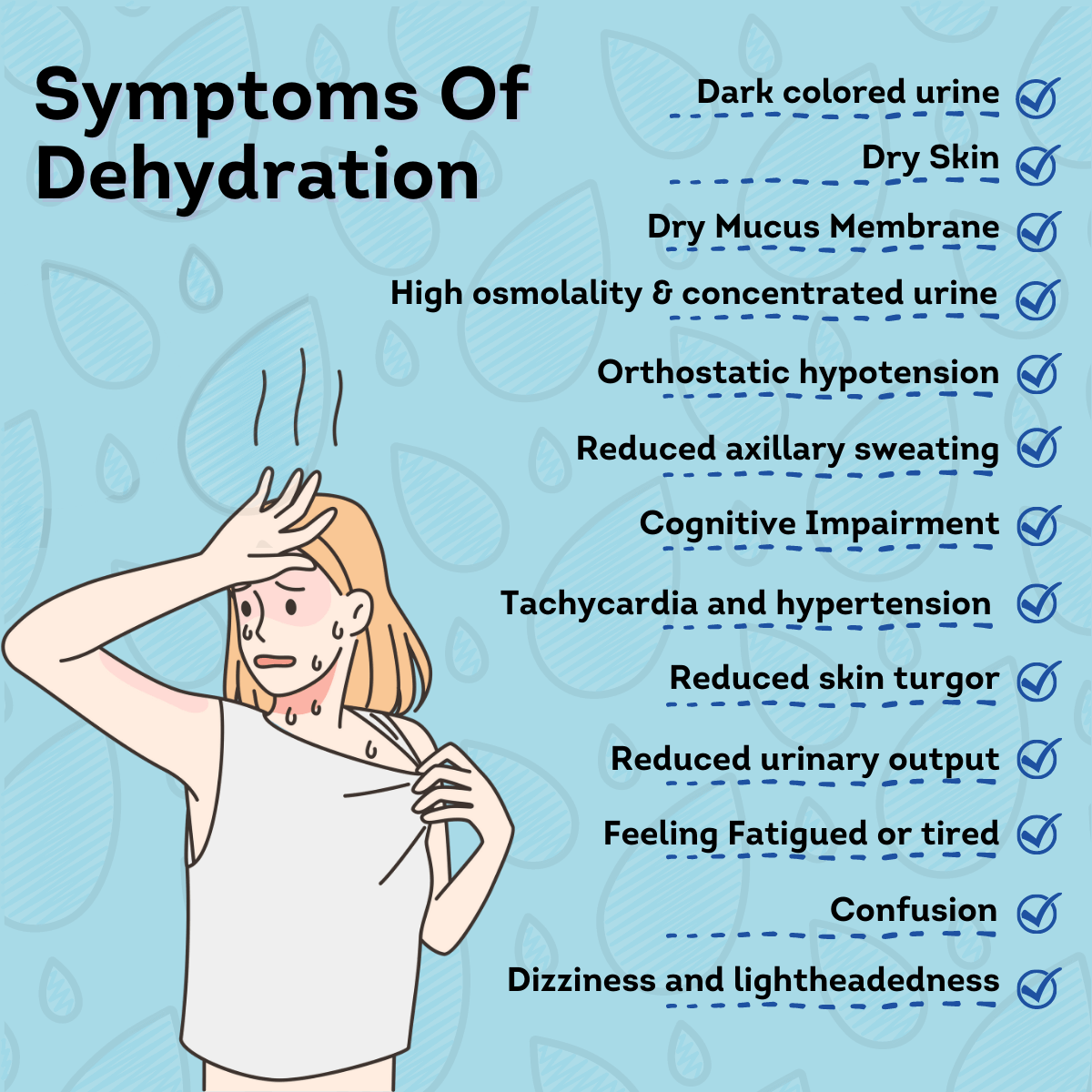
PostCOVID heart palpitations
Many survivors report fluttery feelingsthose rapid, irregular beats that can be unsettling. If you notice a heart rate soaring to 120 beats per minute at rest, that it may signal autonomic dysfunction, and you should get an ECG promptly.
When to call emergency services
Any sudden chest pain, fainting, or severe shortness of breath warrants an immediate 911 call. Remember: its better to be safe than sorryespecially when the heart is involved.
Survival Chances With Heart Disease
If you already live with heart disease, COVID may feel like a grim opponent. But the data is hopeful.
Odds of surviving COVID with a heart condition
According to the American Heart Association, vaccinated individuals with heart disease who contract COVID have a roughly 8590% survival rate, compared with a 7075% rate for the unvaccinated. The vaccines protective effect is evident across age groups and disease severities.
Heart failure COVID19 vaccine benefits
Beyond reducing severe illness, the vaccine appears to lower the incidence of newonset heart failure after infection. A CDC brief published in early 2024 found a 40% drop in postCOVID cardiac complications among those who received a booster dose.
Managing comorbidities
Keeping blood pressure, cholesterol, and blood sugar under control can dramatically improve outcomes. Regular medication reviews with your cardiologistespecially regarding ACE inhibitors or anticoagulantsare key.
Improving Heart Health After COVID
Recovery isnt just about waiting for the virus to go away; its an active process of rebuilding strength and resilience.
Immediate steps (first 30 days)
- Gentle walking or stationary cycling for 1015 minutes, 34 times a day.
- Stay hydratedaim for at least 2L of water daily.
- Prioritize sleep: 79 hours of quality rest supports cardiac repair.
Longterm hearthealthy habits
The Mediterranean dietrich in olive oil, fish, nuts, fruits, and vegetableshas been linked to lower inflammation and better heart function. Swap processed snacks for a handful of almonds or a piece of fresh fruit.
Medical followup schedule
Most cardiologists recommend an echocardiogram at 3 months postinfection, then repeat at 612 months if any abnormalities appear. Blood tests for troponin and BNP can also flag lingering damage early.
When to consider cardiac rehabilitation
If you experience persistent shortness of breath or reduced exercise tolerance, a supervised cardiac rehab program can safely ramp up activity levels under medical supervision. Insurance often covers these programs if a physician prescribes them.
FAQs Quick Answers
Can COVID cause newonset heart failure?
Yes. Ongoing inflammation can weaken the heart muscle even in people with no prior cardiac history.
How long do postCOVID heart symptoms last?
Most people feel better within 36months, but a minority experience symptoms for a year or longer.
Is it safe to get the COVID vaccine if I have heart failure?
Absolutely. Evidence shows vaccinated heartfailure patients have a markedly lower risk of severe outcomes.
What does a heart rate of 120 mean after COVID?
It may indicate autonomic imbalance or dehydration; monitor it and discuss with your doctor if it persists.
Do children develop COVIDrelated heart problems?
Emerging research suggests a slightly increased risk, though the absolute numbers remain low.
Real Stories & Case Studies
A survivors tale
Maria, a 58yearold teacher from Ohio, thought her mild COVID was behind heruntil she started feeling fluttery beats during her morning walks. An urgent echo revealed mild myocarditis. With a month of lowintensity cardio, medication, and a booster shot, Marias heart function returned to baseline. She now shares her story on the Cleveland Clinic blog, encouraging others to listen to their bodies.
Japanese cohort findings
A 2025 UNMC study of 5,000 Japanese patients found that 12% developed some form of cardiac dysfunction within a year of infection, a figure that dropped to 7% among those who were fully vaccinated. The researchers highlighted the importance of early imaging and lifestyle counseling.
Vaccinated vs. unvaccinated outcomes
Table below illustrates the stark contrast in postCOVID cardiac events.
| Group | Heart Failure Incidence (12mo) |
|---|---|
| Fully vaccinated | 4.2% |
| Unvaccinated | 9.8% |
TakeAway Checklist
- Know the top COVID heart damage symptomschest pain, breathlessness, palpitations.
- Schedule a followup echo about 3months after infection.
- Stay uptodate with your COVID19 vaccine and boosters.
- Adopt 150minutes a week of lowimpact cardio (walking, swimming).
- Watch for a resting heart rate >120bpm and call your doctor if it persists.
- Keep blood pressure, cholesterol, and blood sugar in check.
Remember, knowledge is power, but action is what protects your heart. If any of the signs above feel familiar, reach out to your healthcare provider today. And heyif youve navigated COVIDrelated heart issues yourself, share your experience in the comments. Your story could be the encouragement someone else needs.
Take care of that amazing engine inside you. Were all in this together.
FAQs
Can COVID cause new‑onset heart failure?
Yes, the virus can trigger inflammation and clotting that weaken the heart muscle, even in people without prior heart disease.
What are the earliest symptoms of COVID‑related heart failure?
Persistent chest discomfort, shortness of breath with light activity, unusual fatigue, and swelling in the ankles or feet are key warning signs.
How long do post‑COVID heart issues typically last?
Most patients improve within 3‑6 months, though a minority may experience symptoms for a year or longer.
Is it safe to receive a COVID vaccine if I have existing heart failure?
Absolutely. Vaccination markedly reduces the risk of severe COVID and subsequent cardiac complications for heart‑failure patients.
When should I schedule a cardiac follow‑up after COVID infection?
Doctors usually recommend an echocardiogram around three months post‑infection, with additional tests if any abnormalities are found.