Quick answer: Bowelmovement problems in adults can range from a harmless occasional hiccup to serious blockages that need medical attention. Knowing the warning signslike no bowel movement in7days but passing gas or feeling the urge to poop without actually being able tolets you act fast and keep your gut happy.
Why it matters: Your gut is a busy little engine, and when it sputters, youll feel it in every part of your day. Spotting the clues early means you can tweak habits, get the right treatment, and avoid painful complications. Lets dive in together and make sense of whats going on down there.
Understanding the Landscape
What are the most common bowel problems in adults?
Most adults run into at least one of these: constipation, diarrhea, irritable bowel syndrome (IBS), bowel incontinence, and fecal impaction. Roughly 20% of adults experience constipation at some point, and about 10% report chronic diarrhea. These conditions often overlap, so you might notice a mix of symptoms.
How do symptoms differ between men and women?
Women often report more abdominal bloating, pelvic discomfort, and irregular bowel patterns. Hormonal shifts during menstrual cycles, pregnancy, and menopause can also play a role. Thats why youll see specific searches like symptoms of bowel problems in a woman. The core issues are the same, but the triggers can look a little different.
What are serious bowel problems and why they need urgent care?
Serious bowel problems include bowel obstruction, severe fecal impaction, and toxic megacolon. Redflag signs are intense pain, vomiting, inability to pass gas or stool, rapid swelling of the abdomen, and fever. If you notice no bowel movement in7days but passing gas, its a cue to call your doctor sooner rather than later.
How prevalent are bowelmovement issues and whos at risk?
Age, lifestyle, and medical conditions all raise the odds. Sedentary jobs, lowfiber diets, dehydration, certain medications (like opioids or iron supplements), and chronic diseases such as diabetes or hypothyroidism are common culprits. Even pregnancy can tip the balance, making temporary constipation quite normal.
Core Symptoms & When to Worry
What are the classic constipation danger signs?
Watch for fewer than three bowel movements a week, hard or lumpy stools, straining, and a feeling of incomplete evacuation. Some people experience difficulty passing stool but not constipated, which often points to pelvicfloor dysfunction rather than true constipation.
I cant poop but I feel like I have to whats happening?
This is the classic urgefailure cycle. Your rectum sends a signal that its full, but the muscles cant coordinate properly to push. Its common in IBS and in people who spend too much time on the toilet without actually evacuating.
How does no bowel movement in7days but passing gas differ from normal?
Gas can still move through the intestines even when stool is stuck. If youre passing gas but not having a bowel movement for a week, the stool may be hardening or backing upan early sign of obstruction or severe constipation.
What other symptoms signal a deeper issue?
Blood in the stool, unexplained weight loss, nighttime abdominal pain, and a sudden change in stool shape (e.g., thin, pencillike stools) can hint at something beyond routine constipation. If any of these appear, a medical evaluation is wise.
How to use a bowelproblem symptom checker safely?
Online symptom checkers from reputable sites (such as the NHS or Mayo Clinic) can help you decide whether to book an appointment, but theyre not a substitute for professional advice. Think of them as a firststep triage, not a diagnosis.
| RedFlag Sign | Why It Matters |
|---|---|
| No stool for 7+ days (but passing gas) | Possible obstruction or severe impaction |
| Blood in stool | Could indicate hemorrhoids, ulcer, or cancer |
| Sudden change to thin stools | May signal a blockage or colorectal issue |
| Severe, persistent abdominal pain | Risk of bowel perforation or inflammatory disease |
| Fever with abdominal pain | Potential infection or inflammation |
Root Causes Why It Happens
Dietary culprits & quick fixes
Low fiber, inadequate water, and too much dairy or caffeine often nudge your bowels toward trouble. A simple 5step fiber boost can make a world of difference: add a fruit or veggie at every meal, sprinkle seeds on yogurt, swap white bread for whole grain, snack on nuts, and sip water consistently.
Medications that slow the gut
Opioids, anticholinergics, some antidepressants, and iron supplements are common constipationinducing meds. If you suspect a prescription is the cause, talk to your doctor about alternatives or a gentle laxative plan.
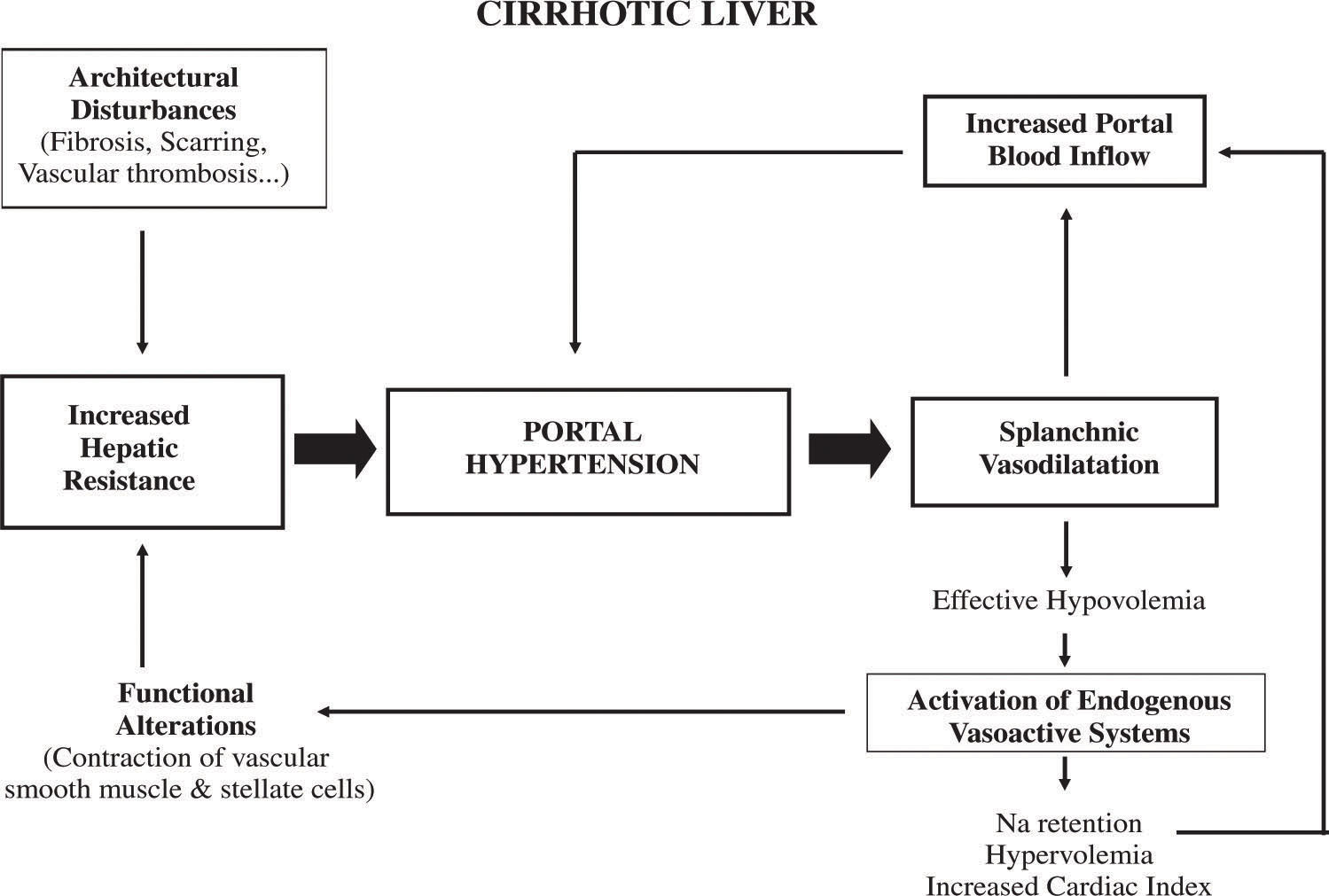
Medical conditions that mimic constipation
IBS, hypothyroidism, diabetes, Parkinsons disease, and even early colorectal cancer can masquerade as simple constipation. Understanding the underlying condition is key because the treatment will differ.
Psychological & lifestyle factors
Stress, anxiety, and an irregular bathroom schedule can disrupt the guts rhythm. Believe it or not, a real messy routinelike rushing to the bathroom after a stressful meetingcan make matters worse. Simple mindfulness or a short walk after meals can reset the pattern.
Agerelated changes
When we get older, the colons muscle tone naturally slows, and we tend to move less. Thats why seniors often need a little extra fiber and hydration. Even a 10minute daily stroll can keep things moving.
When constipation becomes an emergency
Severe pain, vomiting, swelling, or the complete inability to pass gas are emergency signals. In those moments, avoid strong laxatives; call emergency services or head straight to the ER.
Diagnosis Getting the Right Answers
What tests do doctors order?
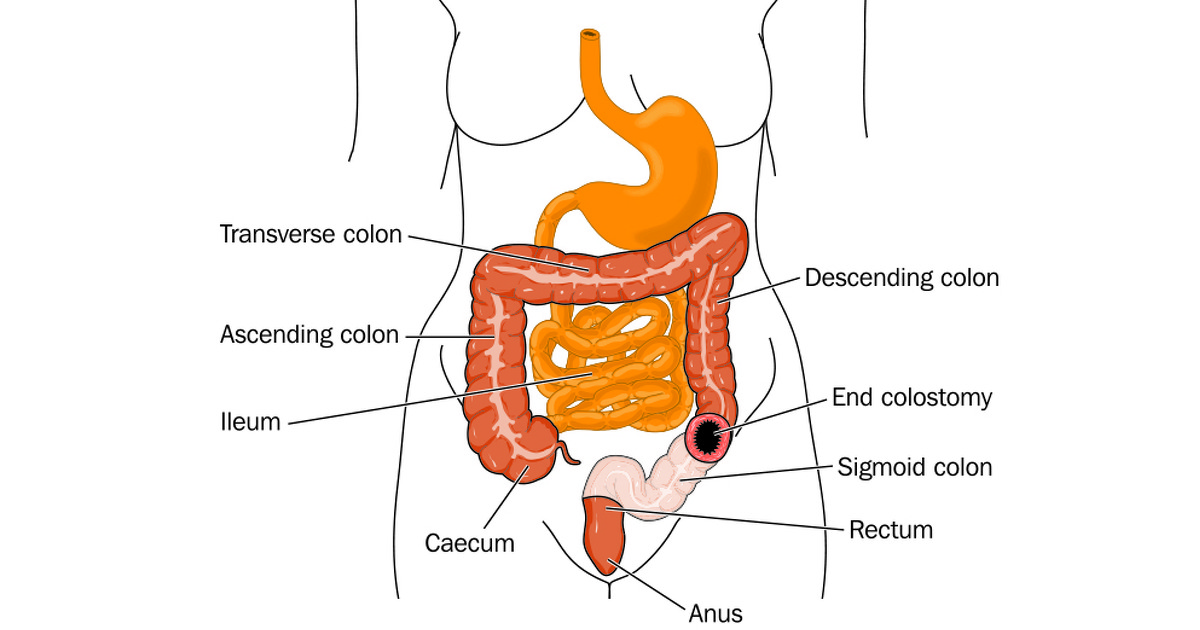
First, a physical exam and a digital rectal exam to feel for blockage. Blood work checks for anemia, thyroid issues, and electrolyte imbalances. Imaginglike an abdominal Xray or CT scanhelps locate any obstruction. A colonoscopy is reserved for persistent or suspicious cases.
How does a bowel problems symptom checker fit in?
Think of it as a friendly nudge. It can guide you toward the right specialist but never replaces a facetoface consultation.
When is a referral to a gastroenterologist needed?
If symptoms linger beyond four weeks, if redflags appear, or if the cause remains unclear after initial tests, a gastroenterologists expertise is essential.
What questions should you ask your GP?
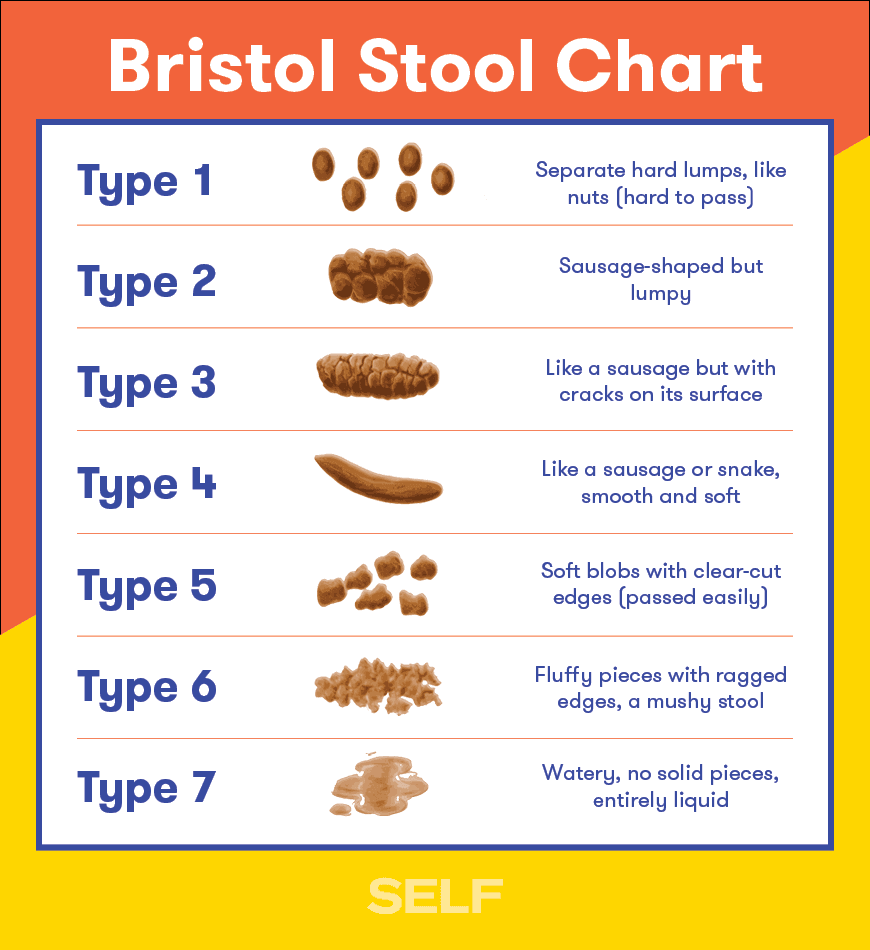
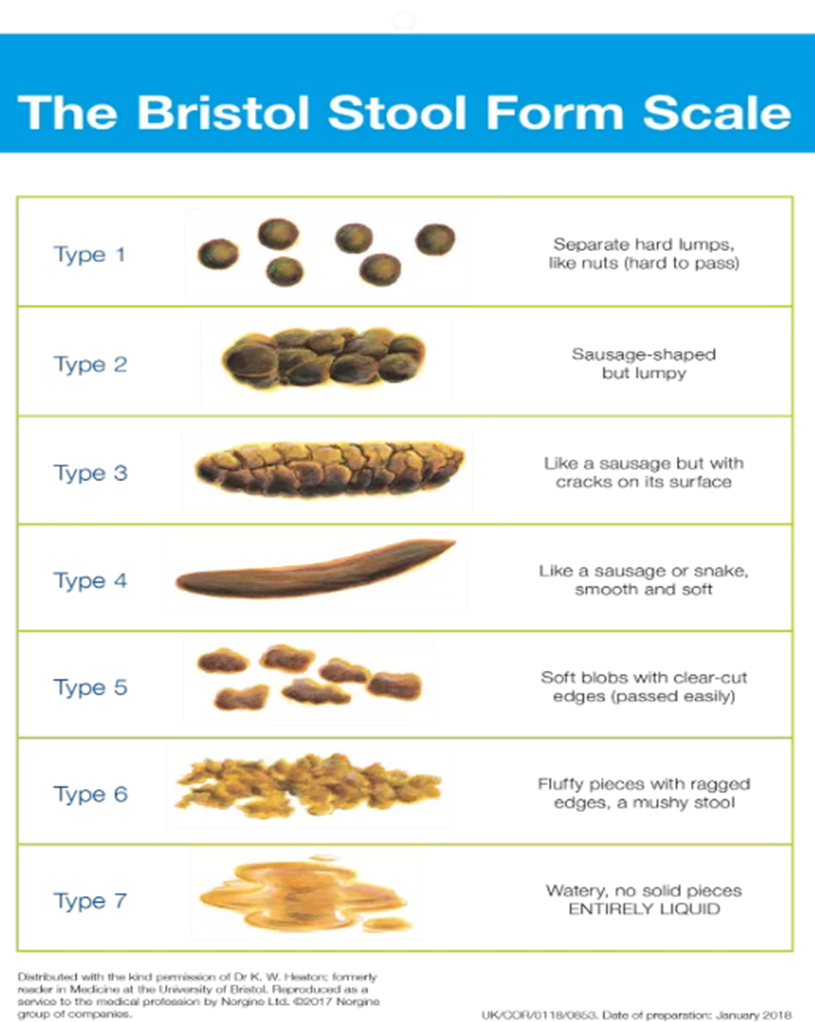
Bring a bowelmovement log (date, stool type using the Bristol chart, any pain). Ask about medication sideeffects, dietary tweaks, and whether a referral is warranted. Knowing the why behind each recommendation builds trust.
Treatment Options From Home Remedies to Medical Care
Firstline lifestyle changes
Start with 2530g of fiber daily, sip at least 2L of water, walk 30minutes a day, and set a regular toilet time after mealsyour body loves routine.
Overthecounter (OTC) aids
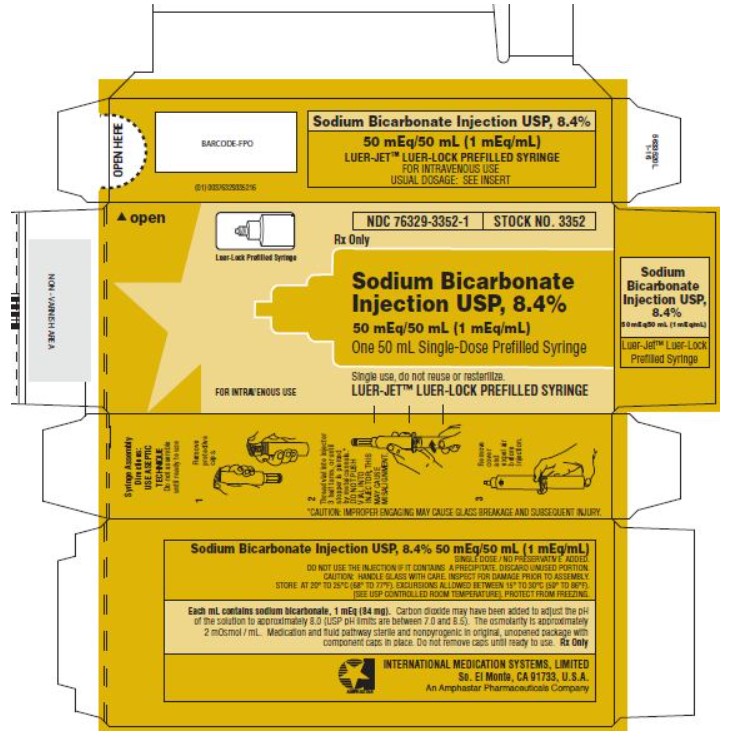
Bulkforming agents like psyllium, osmotic laxatives such as polyethylene glycol, and stool softeners (docusate) are safe for shortterm use. Always follow the label and limit use to a few weeks unless a doctor advises otherwise.
Prescription meds & when theyre needed
Prokinetics, lubiprostone, or linaclotide are options for chronic IBSC. Stimulant laxatives (senna, bisacodyl) are reserved for tougher cases but should not be used daily.
Biofeedback & pelvic floor therapy
If you say, I cant poop but I feel like I have to, pelvicfloor retraining can teach the muscles to coordinate properly. Many find relief after a handful of sessions. For people with specialized pelvic issues, resources on pelvic floor constipation explain common exercises and what to expect from therapy.
When surgery is required
Severe colonic inertia, large fecal impaction, or mechanical obstructions sometimes need an operative approach. Its a last resort after all conservative measures have been explored.
Complementary approaches (with caution)
Probiotics, magnesium citrate, and certain herbal teas (like ginger or peppermint) can help, but evidence varies. A review in the offers a balanced view of what works and whats hype.
How to monitor progress
Keep a simple log: date, time, stool consistency (Bristol chart), and any pain level. Review it with your doctor after two weeks to gauge whether the plan is on track.
Prevention Keeping Your Gut on Track
Build a fiberrich diet that sticks
Think colorful plates: berries, leafy greens, beans, wholegrain pasta, and nuts. A 7day sample plan might start with oatmeal topped with flaxseed for breakfast, a quinoa salad for lunch, and roasted veggies with lentils for dinner.
Hydration hacks for busy adults
Set a reminder to drink a glass of water after each bathroom break. It sounds odd, but the habit pairs fluid intake with the natural urge to go.
Movemore, sitless
Even a 5minute stretch every hour can prevent the gut from getting lazy. Try calf raises while you wait for the coffee to brew.
Routine checkups & screening
Colorectal cancer screening now starts at age 45 for averagerisk adults. Bring up bowel health during your annual physicalyour doctor will appreciate the proactive approach.
Managing stress & mental health
Mindbody practicesyoga, deep breathing, or a quick meditationcan improve gut motility. Its amazing how a calm mind can coax the bowels back into rhythm.
When to seek help early
Keep the constipation danger signs box handy: no stool for 7+ days, blood in stool, severe pain, sudden change in stool shape, fever with abdominal pain. If any appear, call your healthcare provider promptly.
RealWorld Stories & Expert Voices
A day in the life of someone with chronic constipation
Emily, a 38yearold graphic designer, used to dread mornings because shed spend an hour on the toilet with nothing to show for it. After a gentle pelvicfloor physiotherapy program and a fiberboosted diet, she now reports regular, painless movements and a renewed confidence at work.
Interview snippet with a gastroenterologist
Dr. Patel notes, The biggest myth is that holding it in causes permanent damage. While occasional delay is fine, chronic avoidance can weaken the muscles, leading to the urgefailure cycle many describe as I cant poop but I feel like I have to. He recommends a stepwise approach: lifestyle first, then OTC, and finally prescription if needed.
Patientreported success with biofeedback
Mark, a 45yearold accountant, shared his story on a support forum: after three biofeedback sessions, his stuck feeling vanished, and he could finally sit on the porcelain throne without anxiety.
Datadriven case study
A recent study in Gut (2022) showed that participants who followed a structured highfiber regimen plus daily walking reduced constipation episodes by 48% compared to a control group. The numbers underline how simple habit tweaks can make a massive impact.
Conclusion
Bowelmovement problems in adults are more common than most of us admit, but theyre also highly manageable when you recognize the signals early. From the subtle I cant poop but I feel like I have to to the alarming no bowel movement in7days but passing gas, each clue points to a path you can followwhether its a quick diet tweak, a gentle pelvicfloor exercise, or a timely doctors visit. Remember to keep a simple log, stay hydrated, move a bit each day, and never ignore redflag signs.
Take the first step today: track your bowel habits for a week and bring that log to your next appointment. Your gut will thank you, and youll feel more in control of your health. If you have questions or want to share your experience, feel free to reach outlets keep the conversation flowing.