If the pressure in your livers blood vessels starts to climb, you dont have to sit and wait for a disaster there are medicines, lifestyle tweaks, and procedures that can bring that pressure down right now. In the next few minutes well walk through the mosteffective portal hypertension treatment options, show when each is recommended, and flag the biggest prosandcons so you can decide with confidence.
Think of this as a friendly guide rather than a textbook. Ill keep the medical jargon to a minimum, sprinkle in a few realworld stories, and give you a clearcut roadmap you can use today.
Understanding Portal Hypertension
What is portal hypertension?
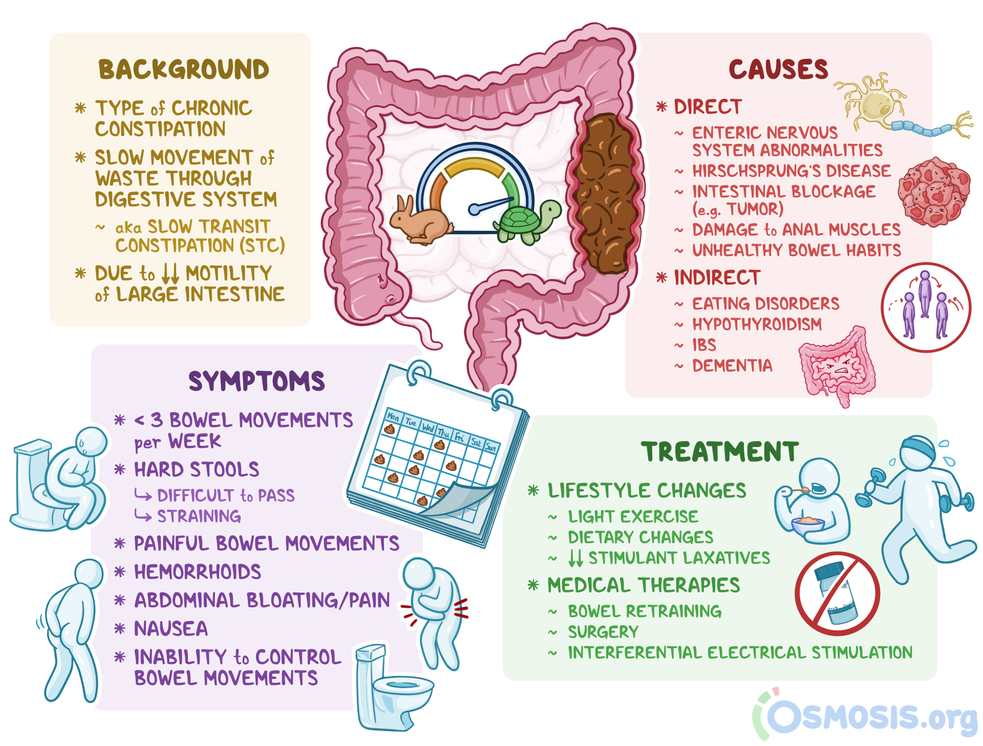
In simple terms, portal hypertension is high blood pressure in the portal vein, the main highway that carries blood from the gut, spleen, and pancreas to the liver. When the liver gets scarred most often because of cirrhosis this highway narrows, and blood backs up, creating a pressure jam.
Why does it usually happen with liver cirrhosis?
Cirrhosis turns healthy liver tissue into stiff scar tissue. That scar tissue contracts the tiny vessels inside the liver, making it harder for blood to flow through. The result? The portal vein gets squeezed, and pressure rises. In fact, most people with portal hypertension have underlying cirrhosis, so youll often hear the phrase liver cirrhosis with portal hypertension treatment.
What stage of cirrhosis is portal hypertension?
Portal hypertension typically appears once cirrhosis reaches the compensated stage the point where the liver can still perform many of its tasks, but the vascular changes have begun. As the disease progresses to decompensated cirrhosis, symptoms become more pronounced and complications rise.
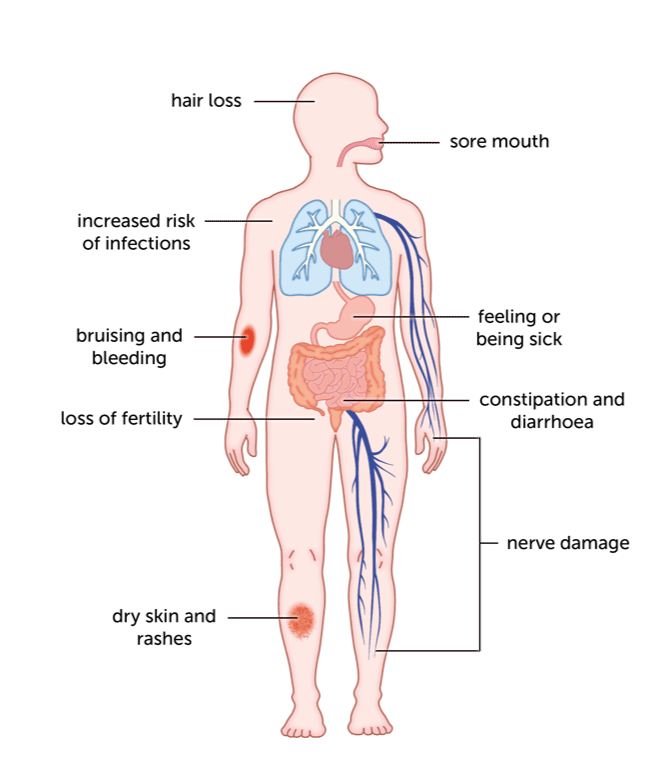
Common portal hypertension symptoms
Most people first notice:
| Symptom | What to Watch For |
|---|---|
| Ascites (fluid buildup) | Sudden belly swelling, weight gain of 2kg in a week |
| Varices (enlarged veins) | Black/tarry stools, vomiting blood |
| Splenomegaly (enlarged spleen) | Feeling full quickly, low platelet count |
| Encephalopathy | Confusion, personality changes |
How is portal hypertension diagnosed?
Doctors usually start with an ultrasound that looks at blood flow, followed by a Doppler study or a CT scan for a clearer picture. The gold standard is measuring the hepatic venous pressure gradient (HVPG) a tiny catheter inserted into a vein to directly gauge pressure. Most patients get the diagnosis through imaging, and the term portal hypertension diagnosis appears in their medical records.
How long can you live with portal hypertension?
Survival depends heavily on the stage of cirrhosis and whether complications like variceal bleeding or severe ascites arise. On average, people with compensated cirrhosis live about 1012years after diagnosis, while those who enter decompensated stages see median survival drop to around 25years. So early treatment really matters.
Can portal hypertension be reversed?
Complete reversal is rare because the scar tissue that caused the pressure jam doesnt magically disappear. However, certain interventions can dramatically reduce pressure and improve quality of life. A liver transplant is the only true cure, but many patients experience lasting relief after procedures like TIPS or effective medication regimens.
FirstLine Treatments
Lowsodium diet
Cutting salt to under 2grams a day (about a teaspoon) is the cornerstone of managing ascites. Studies in the show that strict sodium restriction can reduce fluid buildup by up to 30% within weeks.
Diuretics: spironolactone + furosemide
These two drugs work handinhand: spironolactone blocks aldosterone (the hormone that makes the kidneys hold onto water), while furosemide pushes excess fluid out. The typical starting dose is 100mg of spironolactone with 40mg of furosemide, adjusted based on weight loss and blood work.
Portal hypertension treatment beta blocker
Nonselective betablockers such as propranolol, nadolol, or carvedilol are the first line to lower portal pressure. They do two things: they slow the heart rate (reducing the amount of blood pumped into the portal system) and they cause the blood vessels in the gut to tighten, lowering resistance. Most guidelines suggest a target heart rate of 5560bpm.
| Drug | Typical Dose | Key Benefit | Common Sideeffects |
|---|---|---|---|
| Propranolol | 2080mg twice daily | portal pressure, variceal bleed risk | Bradycardia, fatigue, cold hands |
| Carvedilol | 6.2512.5mg once daily | Strongest pressure reduction | Dizziness, low blood pressure |
Natural treatment portal hypertension
People love the idea of natural fixes. Coffee, modest aerobic exercise, and a balanced plantbased diet may modestly improve liver health, but the evidence is thin. A 2021 review in concluded that no herbal supplement reliably lowers portal pressure. So while a cup of coffee isnt harmful, it shouldnt replace proven meds.
When medication isnt enough
If youre still seeing varices enlarge, ascites persist despite diuretics, or you develop a bleeding episode, its time to talk to your hepatologist about moving on to endoscopic or radiologic therapy.
Procedural Options
Endoscopic variceal ligation (EVL)
During EVL, a gastroenterologist snaps tiny rubber bands onto the swollen veins in the esophagus, causing them to scar and disappear. Its outpatient, painless, and has a 7080% success rate in preventing firsttime bleeds.
Pharmacologic bursts: terlipressin & somatostatin
During an acute bleed, shortacting vasoactive drugs like terlipressin or octreotide (a somatostatin analogue) shrink the portal vessels fast enough to buy time for endoscopic treatment. According to a study in , terlipressin reduces 6week mortality in bleeding patients by roughly 10%.
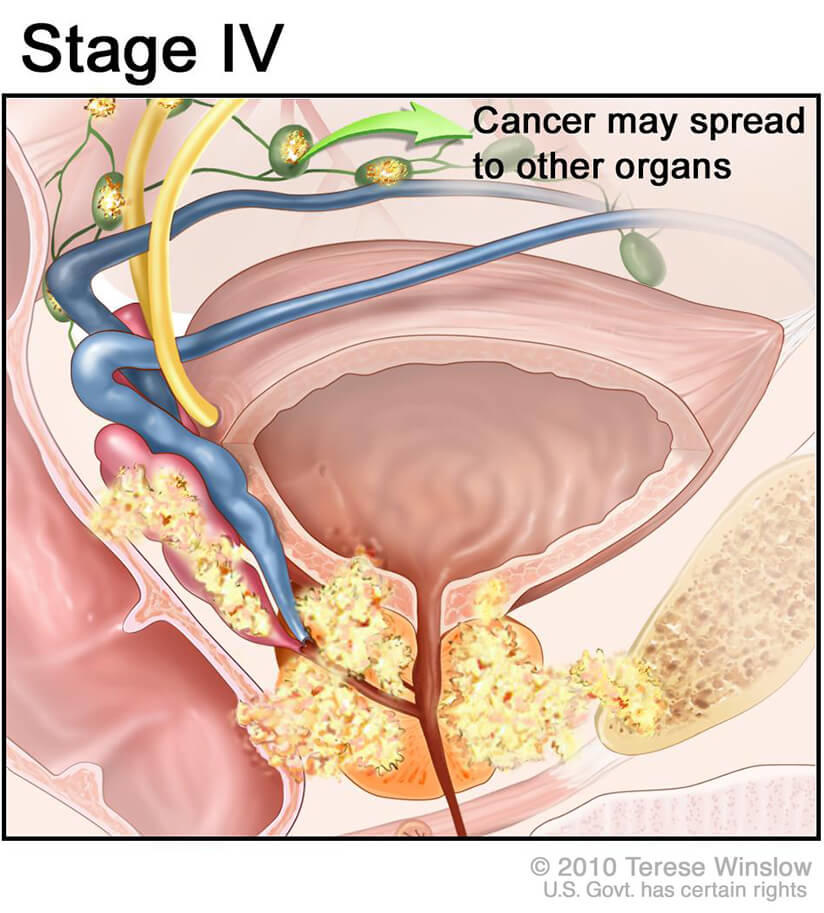
Transjugular intrahepatic portosystemic shunt (TIPS)
TIPS is a radiologyguided tunnel that creates a new pathway for blood to bypass the scarred liver tissue. Think of it as building a sideroad around a traffic jam. It drops portal pressure dramatically, often relieving refractory ascites and preventing further variceal bleeding. The tradeoff is a higher risk of hepatic encephalopathy, so doctors weigh it carefully.
Surgical shunts & liver transplantation
When TIPS isnt an option perhaps due to severe liver failure or clotting disorders surgeons may consider a surgical portocaval shunt. Its a major operation, typically reserved for younger, otherwise healthy patients.
Liver transplantation remains the only definitive cure. Posttransplant, portal pressure normalises, and the underlying cirrhosis disappears. Unfortunately, donor organ scarcity means many patients never get to that point.
Emerging therapies
Researchers are testing novel agents that target the molecular pathways causing vessel constriction, such as endothelin1 antagonists. Early trials look promising, but theyre still years away from routine use.
Managing Risks & Monitoring Progress
Regular labs & imaging
Every 36months, your doctor will check liver enzymes, bilirubin, albumin, and platelet count. Ultrasound every six months helps spot new varices or worsening ascites early.
Watch for medication sideeffects
Betablockers can make you feel sluggish or cause low blood pressure. If your pulse falls below 55bpm or you feel dizzy standing up, let your doctor know a dose tweak often fixes it.
When to call your doctor
Any of the following warrants an immediate call:
- Sudden weight gain >2kg in a week (possible ascites)
- Black or tarry stools (possible GI bleed)
- Severe abdominal pain or swelling
- Confusion, difficulty concentrating
- Rapid heart rate drop after starting a betablocker
Lifestyle habits that may worsen pressure
Alcohol is the biggest enemy even a few drinks a week can accelerate scar formation. Smoking, excessive salty foods, and a sedentary lifestyle also add fuel to the fire. Swapping processed snacks for fresh fruits, walking 2030minutes a day, and staying sober can make a measurable difference.
Support resources
Connecting with others can lift the emotional weight. Organizations like the American Liver Foundation or local portal hypertension support groups provide education, counseling, and a chance to share stories with people who truly understand.
Personalized Roadmap Your StepbyStep Plan
Every patients journey is unique, but most successful plans follow a similar flow:
- Confirm the diagnosis. Get imaging, HVPG (if needed), and baseline labs.
- Start lifestyle changes. Lowsalt diet, alcohol abstinence, light exercise.
- Begin medication. Diuretics plus a nonselective betablocker, unless contraindicated.
- Schedule endoscopic screening. Within six months, an upper endoscopy looks for varices.
- Escalate if needed. If varices are large or bleeding occurs, move to EVL or a pharmacologic burst.
- Consider interventional therapy. Persistent ascites or refractory bleeding may call for TIPS.
- Monitor continuously. Labs, imaging, and symptom journaling keep you and your doctor on the same page.
Visualising this as a flowchart (you could draw it on a napkin) helps you stay on track and discuss each step openly with your hepatologist.
Conclusion
Portal hypertension may feel like a ticking timebomb, but a clear, stepbystep treatment plan from diet and betablockers to advanced procedures like TIPS can keep complications at bay and give you a better quality of life. Whether youre exploring medication, endoscopic therapy, or contemplating a transplant, the key is partnering with a liver specialist who tailors each intervention to your stage of disease and personal goals. If you have questions, experiences to share, or just need a listening ear, drop a comment below or reach out to your healthcare team today. You dont have to face this alone.
For more detailed clinical background on treatment outcomes and diagnosis methods, see this review on portal hypertension diagnosis which summarizes current evidence and diagnostic approaches.
FAQs
What are the first‑line medicines for portal hypertension?
The cornerstone drugs are non‑selective beta‑blockers (propranolol, carvedilol) to lower portal pressure, combined with diuretics such as spironolactone and furosemide to control ascites.
When is a TIPS procedure recommended?
TIPS is considered when patients have refractory ascites, recurrent variceal bleeding, or cannot be controlled with medication and endoscopic therapy.
Can lifestyle changes really affect portal pressure?
Yes. A low‑sodium diet, alcohol abstinence, regular light exercise, and maintaining a healthy weight can lessen fluid buildup and support medical therapy.
What is the role of endoscopic variceal ligation (EVL) in treatment?
EVL is used to eradicate esophageal varices and prevent first‑time or recurrent bleeding. It is usually performed after screening endoscopy shows large varices.
Is liver transplantation the only cure for portal hypertension?
Transplantation is the definitive cure because it replaces the scarred liver, normalising portal pressure. However, many patients achieve long‑term control with medications, lifestyle changes, and procedures like TIPS.