Ever felt a sudden ache in one joint that vanished just as quickly as it appeared, only to show up in another spot a few days later? That jumping pain is what doctors call migratory arthritis, and yes, it can be more than just an annoying nuisance.
In the next few minutes, youll discover what triggers those wandering pains, how long each episode usually sticks around, which conditions it can mimic, and what you can actually dodiet tweaks, meds, lifestyle tipsto feel better faster. Lets get straight to the good stuff, because you deserve clear answers without the fluff.
Quick Facts
What is migratory arthritis? Its a pattern of joint inflammation that moves from one joint to another, typically lasting a few days in each location before hopping again. Unlike chronic arthritis that stays put, this form often resolves on its own once the underlying trigger is addressed.
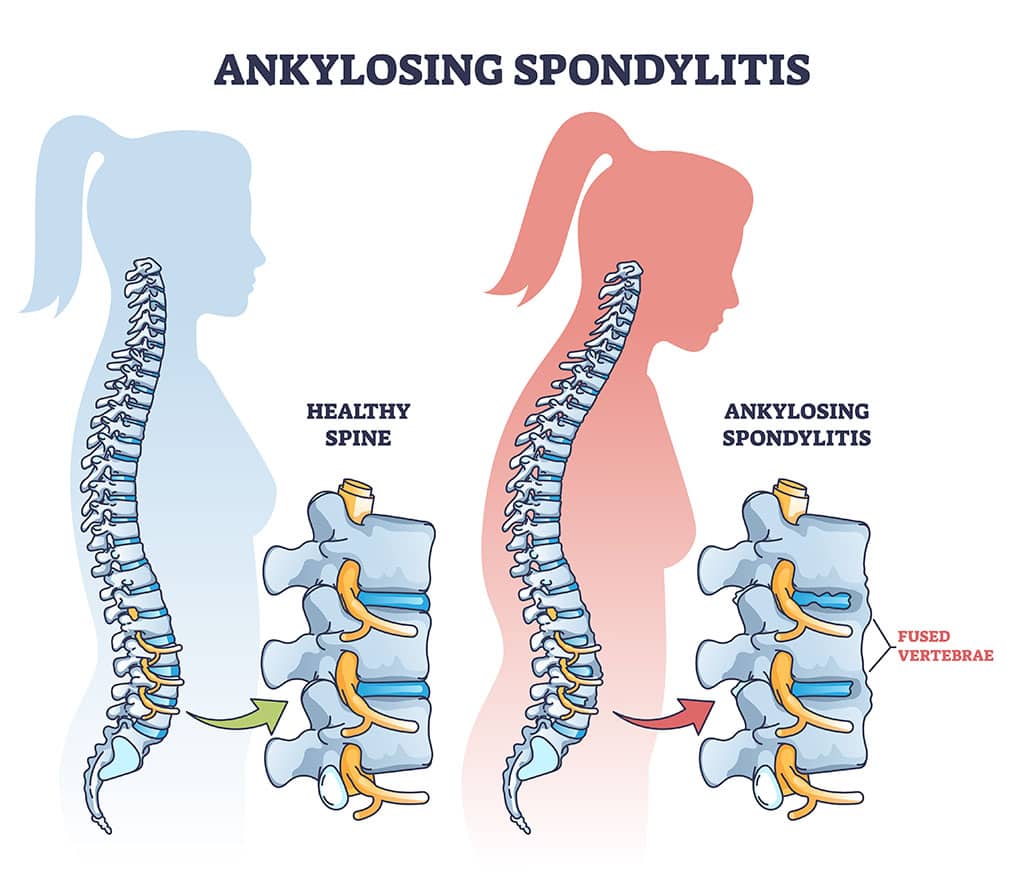
Is it curable? The arthritis itself usually disappears when the cause is treated. If an autoimmune disease is behind it, such as ankylosing spondylitis, you can manage the symptoms and keep flareups at bay through careful monitoring using established AS remission criteria, but the root condition may require ongoing care.
Root Causes
Infectious & PostInfectious Triggers
Several bugs love to set off migratory arthritis. A classic culprit is rheumatic fever, which follows a strep throat infection. Lyme disease, carried by ticks, can also produce a wandering joint pain that mimics other forms of arthritis. In recent years, researchers have documented postCOVID19 inflammatory arthritis, where the virus leaves a lingering jointflare footprint.
Autoimmune & Inflammatory Disorders
Systemic lupus erythematosus (SLE) often includes migratory joint pains along with skin rashes and fatigue. Inflammatory bowel diseaseCrohns or ulcerative colitiscan send the same signals to your joints. Even psoriatic arthritis or ankylosing spondylitis may present with a migratory pattern early on.
LessCommon Triggers
Rarely, certain cancers can masquerade as migratory arthritisa phenomenon known as a paraneoplastic syndrome. Crystalinduced arthritis, like gout, can also hop around, especially in its early stages.
Recognizing Symptoms
Typical Clinical Picture
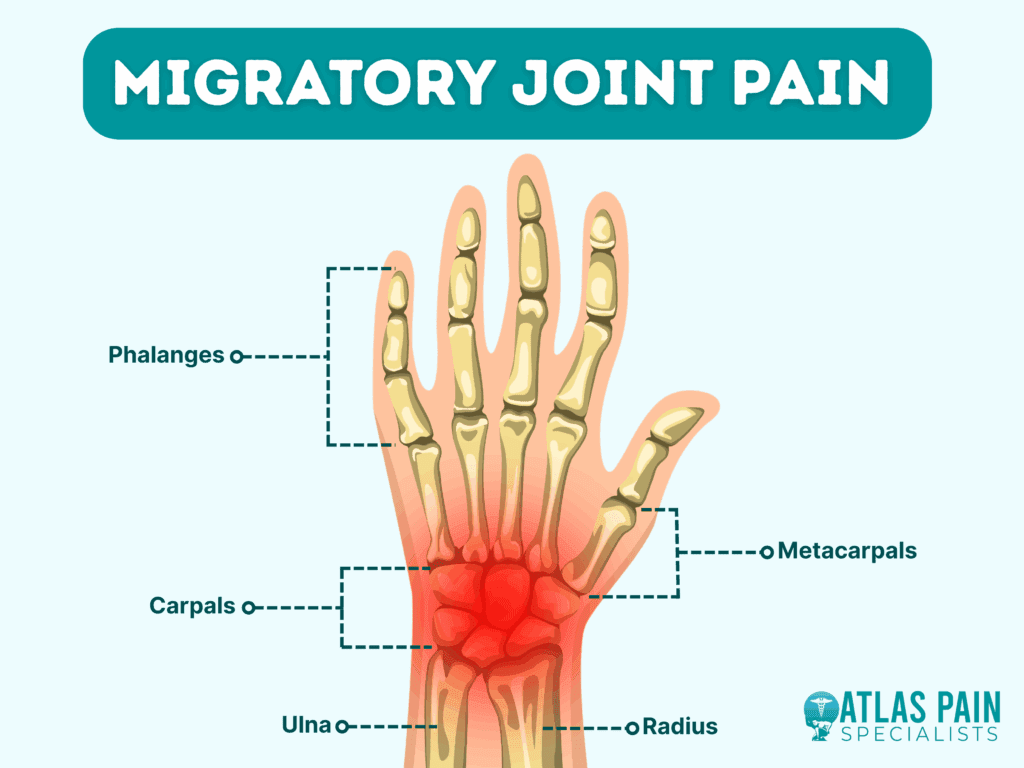
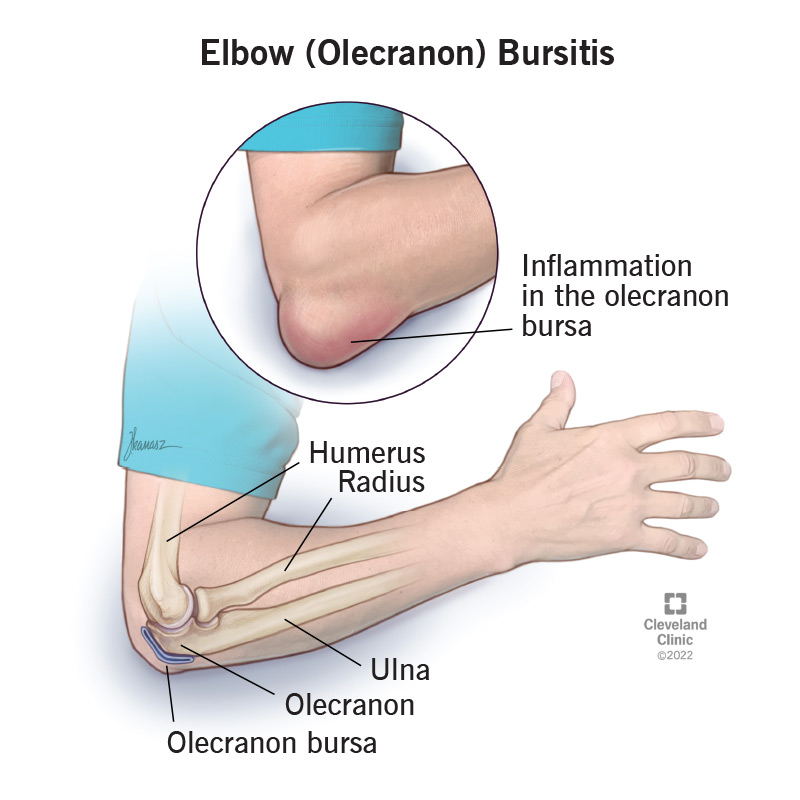
Youll notice sudden swelling, warmth, and tenderness that moves every few days. Commonly affected spots include the knees, wrists, ankles, and elbows. Systemic signs such as lowgrade fever, fatigue, or a faint rash (think lupus) often tag along.
RedFlag Symptoms
If you experience any of the following, call your doctor sooner rather than later:
- Joint swelling that refuses to subside after two weeks.
- Severe pain that stops you from walking or using your hands.
- Unexplained weight loss, night sweats, or a persistent fever.
RealWorld Example
Jane, a 34yearold teacher, thought shed sprained her ankle on a rainy morning. Three days later, her wrist hurt as badly as the ankle did. By the time the pain shifted to her knee, shed Googled migratory joint pain and finally got a referral to a rheumatologist, who diagnosed her with poststreptococcal arthritis.
How Long Lasts
Acute Episodes vs. Chronic Patterns
Each joint typically chafes for 37days. A full episodewhere the pain jumps through a few jointsusually resolves within 24weeks. However, if the underlying disease (like lupus) flares up again, the migratory pattern can recur.
Timeline Visual (Suggested)
Imagine a simple chart: Day03ankle, Day47wrist, Day812knee, and so on. This visual helps you track when a new joint joins the party.
Diagnosis & Differential
Lab WorkUp
Doctors start with a blood panel: CBC, ESR/CRP for inflammation, ANA and dsDNA if lupus is suspected, and rheumatoid factor (RF) or antiCCP to rule out rheumatoid arthritis. If a tick bite is in the history, Lyme serology is ordered. For postCOVID cases, a COVID19 antibody test may be added.
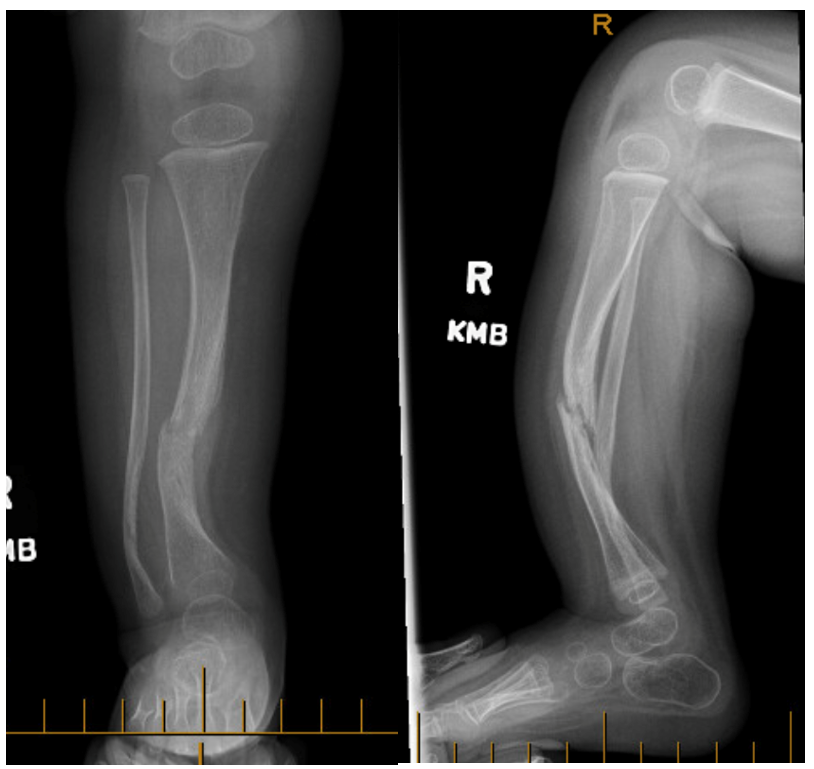
Imaging
Plain Xrays rule out bone erosion. An ultrasound can spot fluid in the joint and differentiate crystal deposits from pure inflammation.
Migratory Arthritis Differential
| Condition | Key Distinguishing Feature | Typical Labs |
|---|---|---|
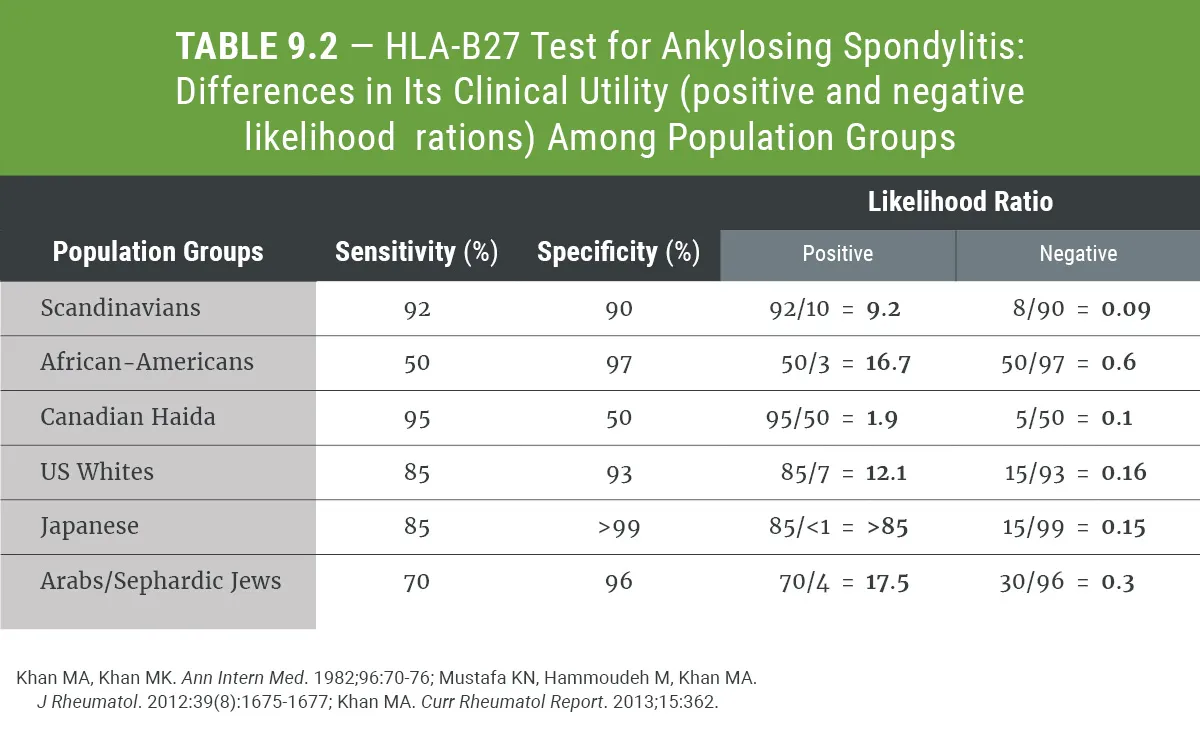
| Reactive arthritis | Follows GI or GU infection | HLAB27 positive |
| Rheumatoid arthritis | Symmetrical, persistent involvement | RF+, antiCCP+ |
| Gout/pseudogout | Sudden monoarthritis, crystal analysis | Synovial fluid crystals |
| Paraneoplastic polyarthritis | Cancer history, weight loss | Variable, tumor markers |
For deeper insight, you can read a recent review in NEJM that discusses postCOVID joint inflammation.
Treatment Options
Treat the Underlying Cause
If an infection is responsible, a targeted antibiotic (e.g., doxycycline for Lyme disease) is the first step. Autoimmune triggers often need diseasemodifying antirheumatic drugs (DMARDs) such as methotrexate, and in stubborn cases, biologics that block TNF.
Symptomatic Relief
Nonsteroidal antiinflammatory drugs (NSAIDs) like ibuprofen or naproxen are the goto for pain and swelling. When flares roar louder, a short course of oral prednisone or a single intraarticular steroid injection can calm the storm.
Lifestyle & Diet
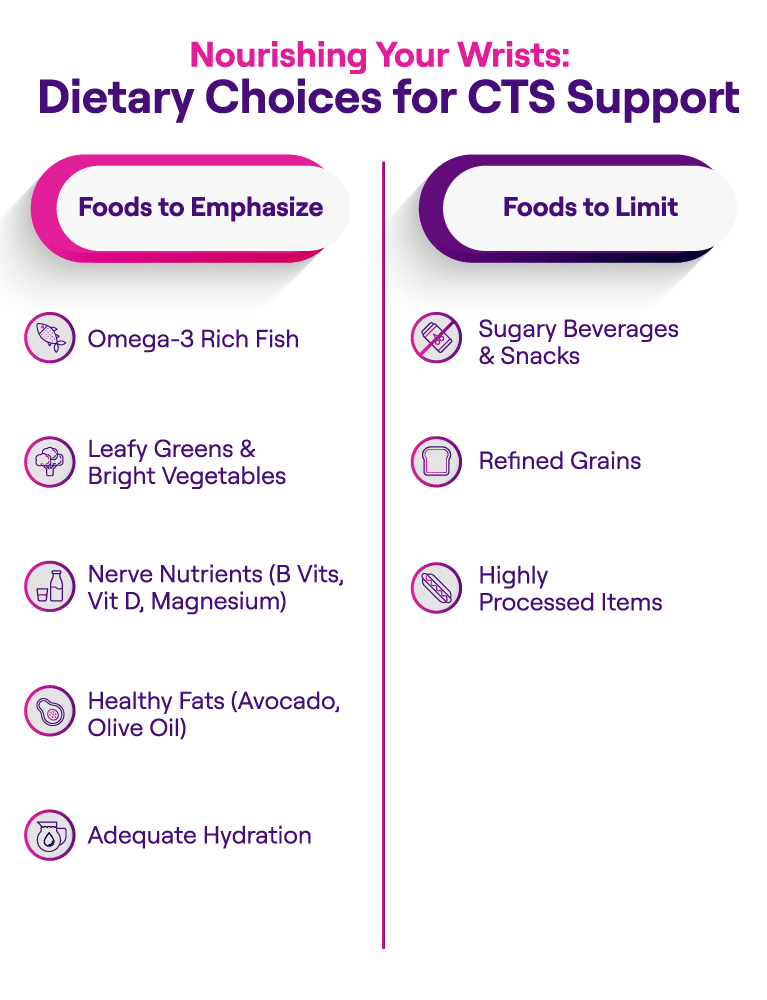
While food wont cure the root cause, an antiinflammatory diet can soften the edges:
- Omega3rich fish (salmon, sardines) a few times a week.
- Leafy greens, berries, and nuts for antioxidants.
- Turmeric or ginger teas for a gentle spiceboost.
- Limit processed sugars and refined carbs, which can fan inflammation.
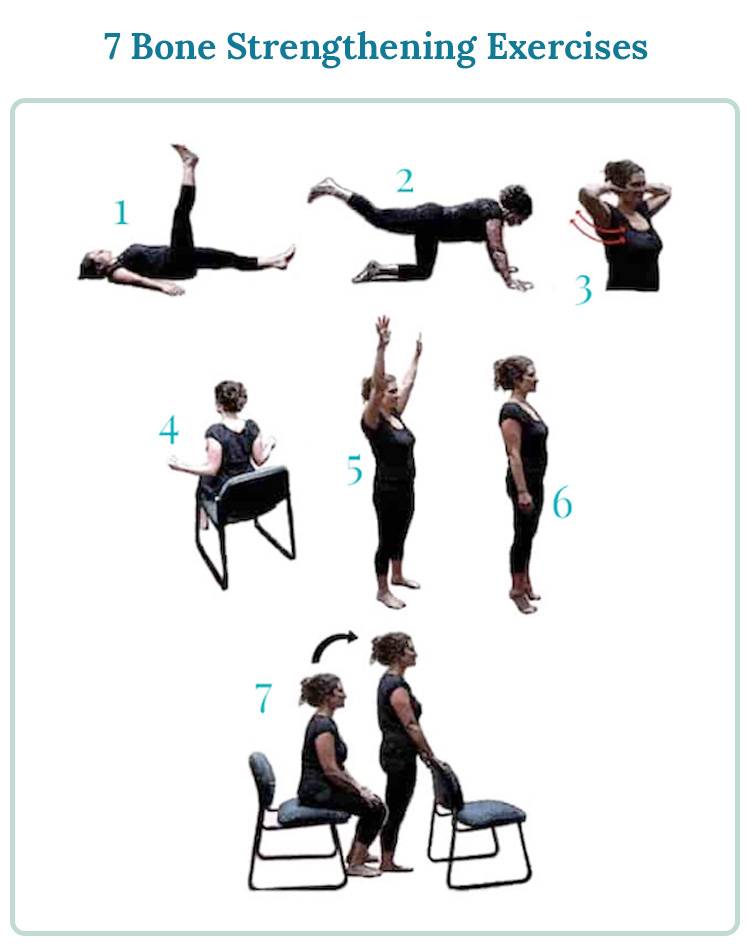
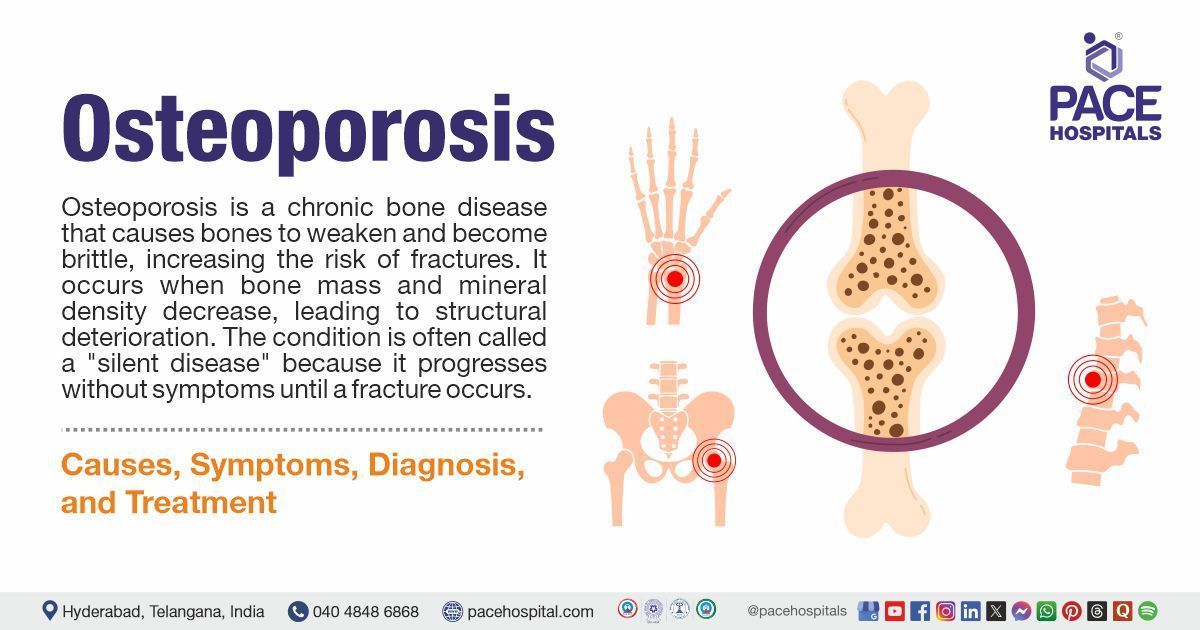
Staying hydrated and maintaining a healthy weight also reduces stress on your joints. Gentle rangeofmotion exerciseslike a 10minute daily walk or water aerobicskeep joints lubricated without overloading them. For those with related bone concerns, osteoporosis physical therapy and specific osteoporosis exercises can complement joint health and overall mobility.
QuickTips Box
What you can do today:
- Apply an ice pack to the painful joint for 15minutes, three times a day.
- Take ibuprofen 400mg with food, as needed for pain.
- Start a short, lowimpact walkjust 10minutesto keep blood flowing.
- Add a tablespoon of ground flaxseed to your morning smoothie for omega3s.
When to Seek Care
Urgent attention is needed if you have high fever, severe swelling that prevents movement, or sudden inability to bear weight. For routine evaluation, schedule an appointment if joint pain hops around for more than two weeks or if youre unsure whats causing it.
A typical followup plan looks like this: initial visit lab work & imaging reassessment in 46weeks to see how the treatment is steering the symptoms.
Summary
Migratory arthritis may feel like a mystery guest who shows up uninvited, moves from room to room, and leaves you guessing. The good news? Most episodes are shortlived, and identifying the triggerwhether its a lingering infection, an autoimmune flare, or even a postCOVID reactionlets you target the problem directly. By pairing proper medical care with simple lifestyle tweaksa balanced antiinflammatory diet, gentle movement, and timely pain reliefyou can keep those wandering aches from crashing your day.
If youve experienced joint pain that seems to bounce around, consider downloading our free Migratory Arthritis Symptom Tracker to log your flares and share them with your doctor. And remember, you dont have to navigate this alonereach out, ask questions, and let the right support guide you back to comfort.
FAQs
What exactly is migratory arthritis?
Migratory arthritis is a pattern of joint inflammation that moves from one joint to another, typically lasting a few days in each spot before shifting.
Which conditions most often cause migratory arthritis?
Common triggers include post‑streptococcal (rheumatic fever), Lyme disease, reactive arthritis after infections, systemic lupus erythematosus, and lately post‑COVID‑19 inflammatory arthritis.
How long does an episode of migratory arthritis usually last?
Each affected joint usually hurts for 3‑7 days, and the entire series of flares often resolves within 2‑4 weeks if the underlying cause is treated.
What tests are used to diagnose migratory arthritis?
Doctors typically order blood work (CBC, ESR/CRP, ANA, RF, anti‑CCP, Lyme serology) and may use X‑rays or joint ultrasound to look for fluid or crystal deposits.
What treatments can relieve the pain and stop the migration?
Treatment targets the cause: antibiotics for infections, DMARDs or biologics for autoimmune disease, and NSAIDs or short courses of steroids for symptom relief, plus lifestyle measures like an anti‑inflammatory diet and gentle exercise.