Hey there, friend. If youve just heard the words esophageal perforation and feel your heart start to race, youre not alone. Its a scary phrase, but the good news is that getting the right diagnosis right away can make all the difference between a smooth recovery and a serious complication. Below, Ill walk you through exactly what to look for, which tests really help, and how doctors decide on the best treatmentwithout any jargonfilled fluff.
When to Suspect
What are the telltale symptoms?
Sudden, sharp chest or neck pain that feels like a knifestabbing is often the first clue. You might also notice:
- Difficulty swallowing (dysphagia) or the feeling that food is stuck
- Subcutaneous emphysemaair bubbling under the skin that makes a crackling sound when you press on it
- Fever, chills, rapid heartbeat, or low blood pressure
These signs are especially common after an endoscopy, forceful vomiting, or blunt chest trauma. In other words, if youve just had an upper GI procedure and start feeling this way, treat it as an emergency.
Why does timing matter?
Doctors talk about the golden 24hour window. A study published in showed mortality drops from 30% to under 10% when a perforation is identified within the first day. Thats why quick recognition is the cornerstone of esophageal perforation diagnosis.
FirstLine Imaging
Chest Xray: What can it actually show?
A plain chest Xray is often the first test because its fast and widely available. Look for:
| Finding | What it Means |
|---|---|
| Free air under the diaphragm | Leak of air from the esophagus into the abdomen |
| Mediastinal emphysema | Air trapped in the central chest cavityclassic for perforation |
| Pleural effusion (fluid) | Possible infection spreading into the chest lining |
These esophageal perforation Xray findings are indirect, so a normal Xray doesnt completely rule out a tear.
Contrast Esophagography: The definitive test
When the Xray raises suspicion, the next step is a contrast swallow study. Two types of contrast are used:
- Watersoluble contrast (Gastrografin) safer if a leak is present because its less irritating to the mediastinum.
- Barium sulfate more sensitive, but can cause a severe inflammatory reaction if it escapes.
Guidelines suggest starting with watersoluble contrast; if the study is negative but clinical concern remains high, a followup barium study can be performed. The leak will typically appear as a spillage of contrast outside the esophageal lumen.
CT Scan with Oral/IV Contrast: The gold standard
CT imaging, especially with oral contrast, gives a 3dimensional view of the leak, surrounding fluid collections, and any mediastinal infection. Its also the best tool for planning surgery.
Key CT clues include:
- Extraluminal air tracking along the esophagus
- Contrast extravasation into the mediastinum or pleural space
- Localized fluid collections or abscesses
According to , CT has a sensitivity of over 90% for detecting esophageal perforations.
Endoscopic Tests
Is diagnostic endoscopy safe?
Endoscopy lets a physician see the tear directly and even place a covered stent for immediate sealing. However, inflating the scope can worsen a small perforation, so its usually reserved for cases where imaging is inconclusive or when the team plans an endoscopic repair.
What labs help?
Blood work isnt diagnostic, but it tells you how severe the situation is. Typical findings include:
- Elevated white blood cell count (leukocytosis)
- High lactate levels indicating tissue hypoxia
- Acidbase disturbances on arterial blood gas
These labs guide urgencyhigher lactate often means a bigger infection risk.
Decision Making
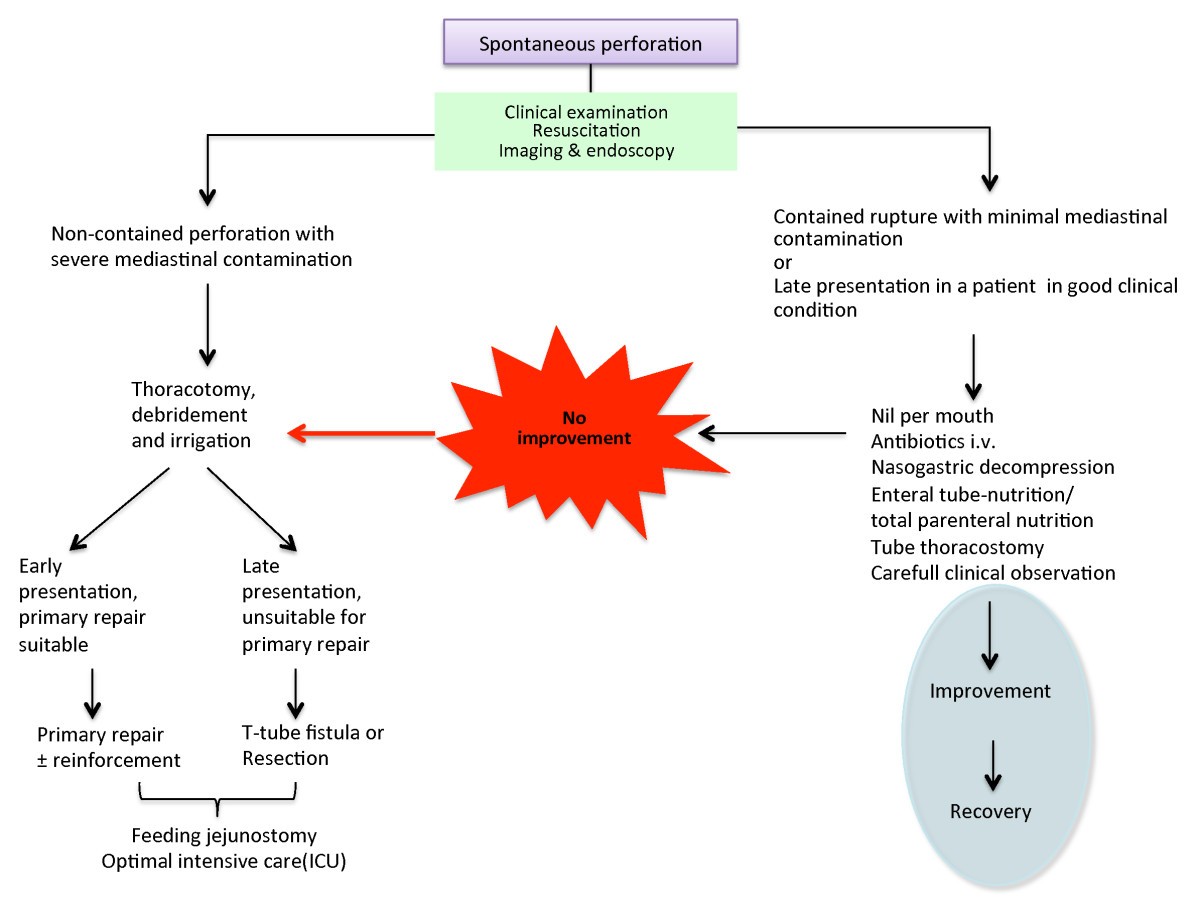
How do doctors decide on treatment?
Several factors shape the final plan:
- Location of the tear cervical (neck) leaks are more likely to be managed conservatively, while thoracic (chest) perforations often need surgery.
- Size of the leak small leaks (<10mm) may seal with antibiotics and fasting; larger defects usually require repair.
- Time since injury under 24hours favors primary repair; beyond 48hours, contamination may demand drainage and possibly esophageal diversion.
What are the main treatment options?
Conservative management includes nil per os (NPO), broadspectrum IV antibiotics (e.g., piperacillintazobactam), and close monitoring. Its ideal for tiny cervical perforations diagnosed early.
Endoscopic repair uses selfexpanding metal or plastic stents to seal the defect. This approach grew popular after a 2022 multicenter trial showed comparable success to surgery for leaks <2cm.
Esophageal perforation surgery ranges from primary repair (suturing the tear) to more complex procedures like esophagectomy in severe cases. The decision matrix is often displayed as a flowchart in surgical textbooks.
Pitfalls & Complications
Why can imaging miss a leak?
Early CT scans performed before oral contrast reaches the tear can look normal. Small cervical perforations may not generate enough air to be seen on plain Xray. Thats why a repeat study 1224hours later is recommended when suspicion stays high.
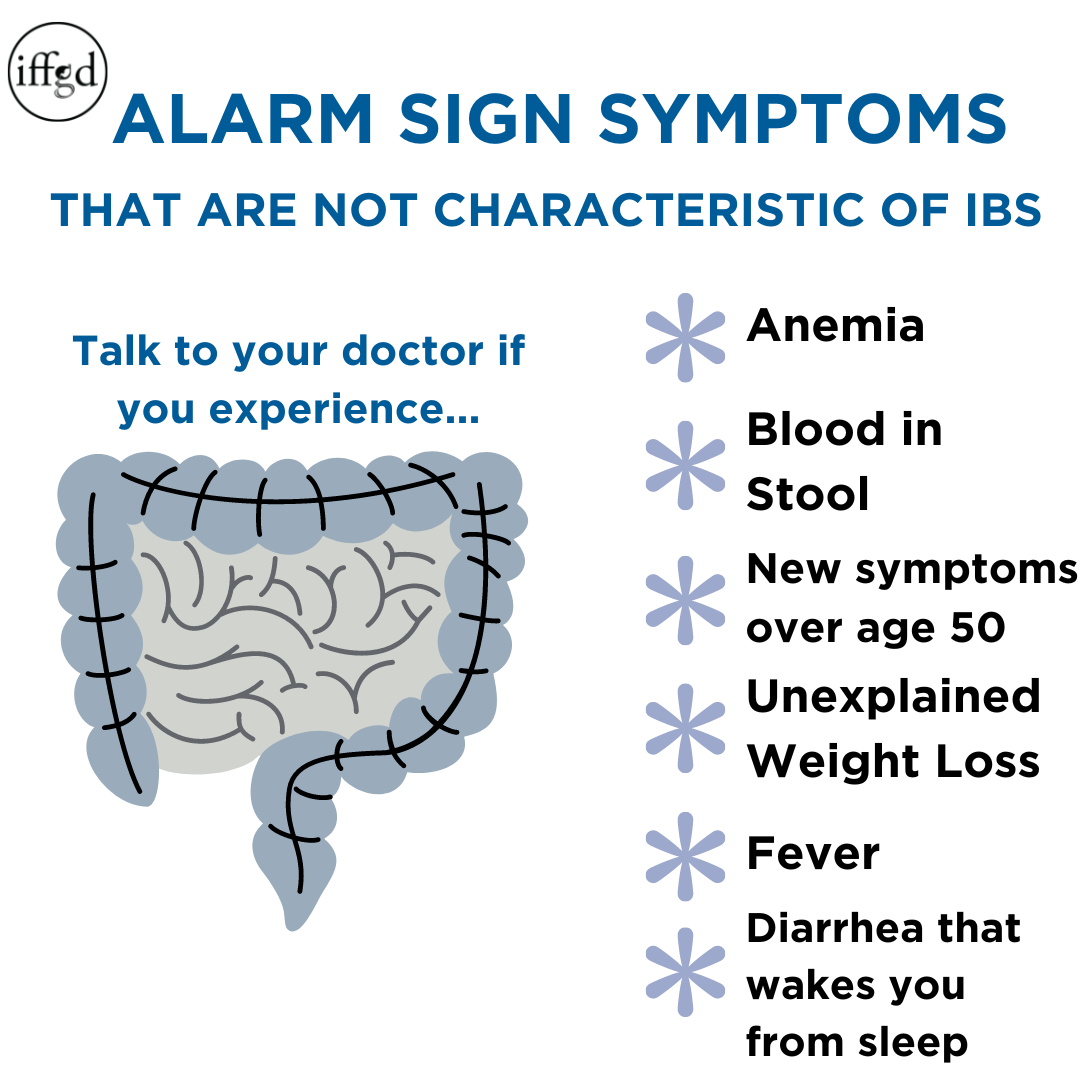
What complications should I watch for?
Even with prompt diagnosis, the following esophageal perforation complications can arise:
- Mediastinitis infection of the central chest cavity, a lifethreatening condition.
- Empyema pus collecting in the pleural space, often needing drainage.
- Sepsis systemic infection, which can lead to organ failure.
- Stricture formation scar tissue narrowing the esophagus, sometimes requiring dilation later on.
And yes, you may wonder, Can you die from a ruptured esophagus? Unfortunately, the answer is yesespecially when diagnosis is delayed beyond 48hours. Thats why the golden window matters so much.
Recovery & Followup
How long does healing take?
Recovery time varies:
- Uncomplicated, conservatively managed perforations often heal in 24weeks.
- Patients who undergo esophageal perforation surgery may need 612weeks before returning to normal diet.
- Those with endoscopic stent placement usually keep the stent for 46 weeks before removal.
During this period, youll have frequent chest Xrays or CT scans to ensure the leak is sealing and that no new collections are forming.
What should I do at home?
Heres a quick checklist to keep you on track:
- Stay NPO until your doctor says its safe to start liquids.
- Take antibiotics exactly as prescribed. Skipping doses can let infection creep back.
- Watch for warning signsincreasing chest pain, fever, shortness of breath, or a new cough.
- Follow nutritional guidance. Many centers provide highcalorie, lowvolume feeds through a feeding tube while your esophagus rests.
- Attend all followup appointments. Imaging will guide when you can safely chew again.
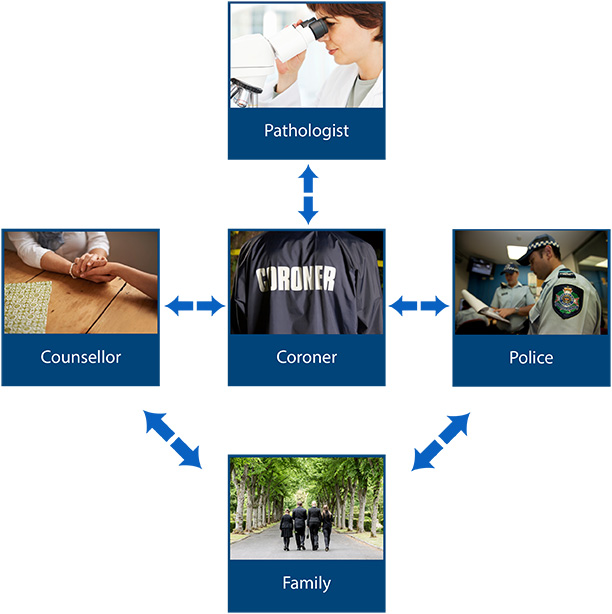
Putting It All Together
Getting an esophageal perforation diagnosis is a race against time, but its also a story of teamworkbetween you, your emergency doctors, radiologists, surgeons, and sometimes endoscopists. Recognize the redflag symptoms, push for the right imaging (especially a contrast study or CT), and stay engaged in the decisionmaking process.
Remember, early detection dramatically lowers the risk of severe esophageal perforation complications and shortens the recovery time. Whether you end up with a short course of antibiotics, a stent, or an operation, the goal is the same: seal the leak, control infection, and get you back to enjoying a normal meal without fear.
Have you or someone you know gone through this? What was the most confusing part of the diagnosis or treatment? Share your story in the commentsId love to hear how you navigated the journey. And if you have any lingering questions, feel free to ask; were all in this together.
Take care, stay vigilant, and remember that the sooner you get the right diagnosis, the brighter the road to recovery.
FAQs
What are the most common signs of an esophageal perforation?
Typical clues include sudden, sharp chest or neck pain, difficulty swallowing, subcutaneous emphysema (a crackling sensation under the skin), fever, chills, rapid heartbeat, and low blood pressure, especially after endoscopy, forceful vomiting, or chest trauma.
Which imaging test is considered the gold standard for detecting an esophageal perforation?
A contrast‑enhanced CT scan of the chest (with oral and IV contrast) is the gold standard because it shows extraluminal air, contrast leak, fluid collections, and guides surgical planning with >90 % sensitivity.
When should water‑soluble contrast be used instead of barium for an esophagogram?
Water‑soluble contrast (Gastrografin) is preferred initially when a leak is suspected because it is less irritating to mediastinal tissues. If the study is negative but clinical suspicion remains high, a follow‑up barium study can improve detection.
How does the timing of diagnosis influence treatment options?
Diagnosis within the first 24 hours usually allows primary surgical repair or endoscopic stenting. Perforations identified after 48 hours often require drainage, possible esophageal diversion, and more extensive infection control measures.
Can a small esophageal perforation be managed without surgery?
Yes. Small cervical leaks (<10 mm) diagnosed early can be treated conservatively with nil per os (NPO), broad‑spectrum IV antibiotics, close monitoring, and nutritional support, often avoiding operative intervention.