Feeling like your bowels have decided to take an extended vacation? If you're battling stubborn, infrequent stools, bloating, or that nagging ache in your lower belly, you're likely dealing with chronic constipationa lingering problem that can affect anyone.
In the next few minutes, we'll uncover why it happens, the warning signs you shouldn't ignore, and a step-by-step plan (including lifestyle tweaks and medical options) that can finally put an end to the discomfort for good.
What Is Chronic Constipation
Definition & Diagnostic Criteria
Medically, chronic constipation is defined as bowel movements that occur fewer than three times per week, with hard or pellet-like stools, persistent straining, or a feeling that you haven't completely emptied the bowelsand the condition lasts at least three months. The criteria help doctors distinguish it from occasional, short-term constipation.
How It Differs From Occasional Constipation
Everyone gets stuck now and then after a night of pizza, but chronic constipation sticks around. It's not just about frequency; it's about the impact on daily lifemissed work, discomfort, and even anxiety about using the bathroom.
Quick FAQ (FeaturedSnippet Ready)
| Question | Answer |
|---|---|
| What is chronic constipation? | A bowel-movement problem lasting 3 months, with hard or pellet-like stools, straining, or a feeling of incomplete evacuation. |
Common Causes & Risks
General Causes (The Why)
Below are the most frequent culprits, pulled from a comprehensive review:
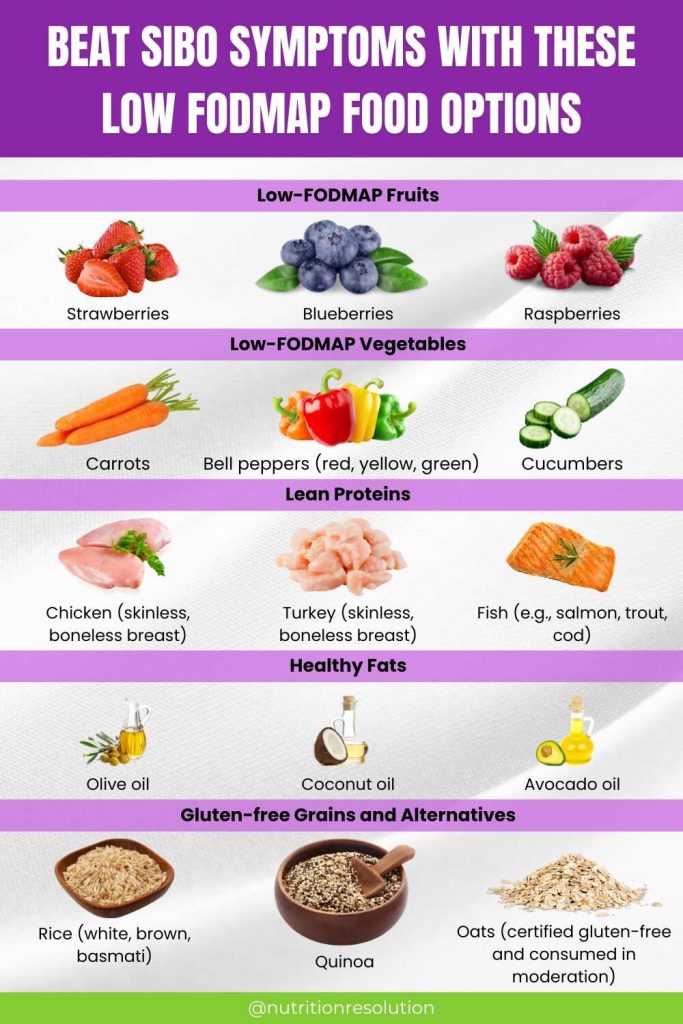
- Low-fiber dietnot enough fruits, veggies, whole grains.
- Insufficient water intakedehydration makes stool hard.
- Sedentary lifestylelack of movement slows down gut motility.
- Medicationsopioids, antacids, some antidepressants.
- Thyroid disordersespecially hypothyroidism.
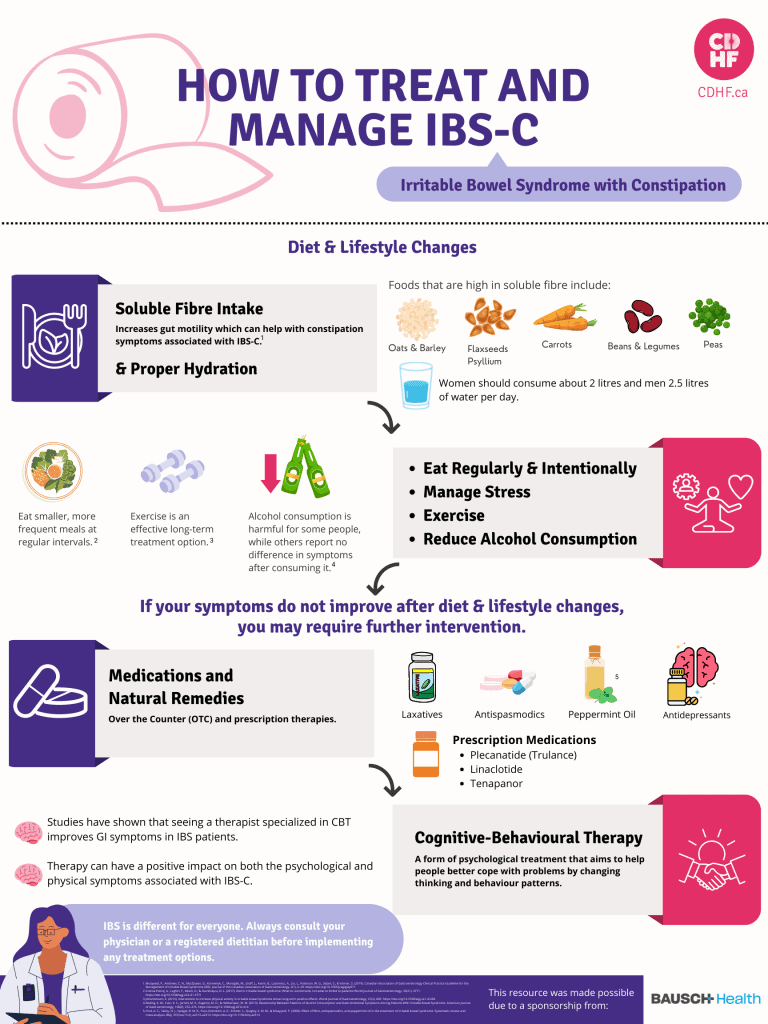
- Irritable bowel syndrome (IBS)disrupts normal rhythm.
- Depression & stressaffect the brain-gut connection.
- Neurological diseasesParkinson's, multiple sclerosis.
Causes of Constipation in Women
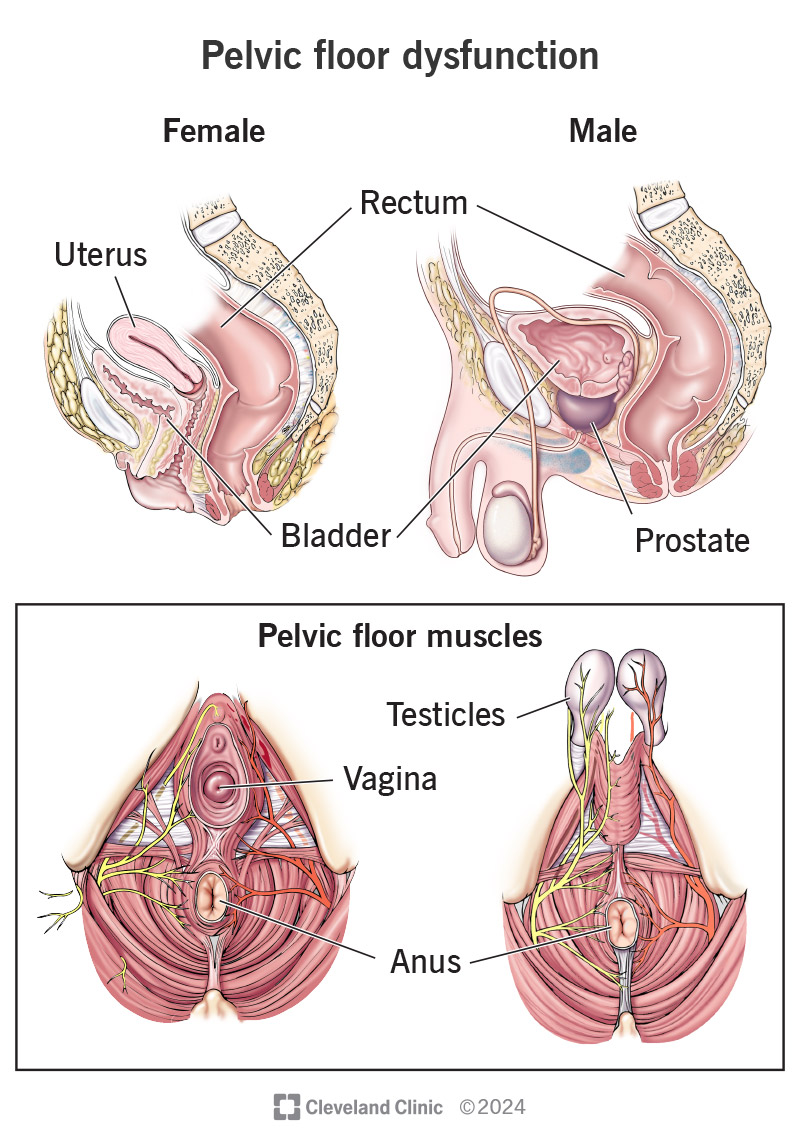
Women face a few extra hurdles. Hormonal fluctuations during menstrual cycles, pregnancy, and menopause can all relax the pelvic floor muscles, making stool passage trickier. Additionally, conditions like endometriosis can cause pelvic pain that interferes with normal bowel habits.
Medical Conditions & ICD10 Code
When a doctor logs your diagnosis, chronic constipation appears in the ICD10 system as K59.0. This code links the condition to underlying diseases such as diabetes, Parkinson's, or chronic kidney disease, each of which can alter gut motility.
Comparison TableLifestyle vs. Medical Triggers
| Trigger Type | Example | Typical Influence on Bowel Motility |
|---|---|---|
| Lifestyle | Low fiber intake | Slows transit time |
| Medication | Opioids | Direct muscle relaxation |
| Disease | Hypothyroidism | Alters hormonal signaling |
Danger Signs to Watch
Constipation Danger Signs Checklist
Most of us ignore small red flags until they turn serious. Keep an eye out for any of the following and consider a prompt medical visit:
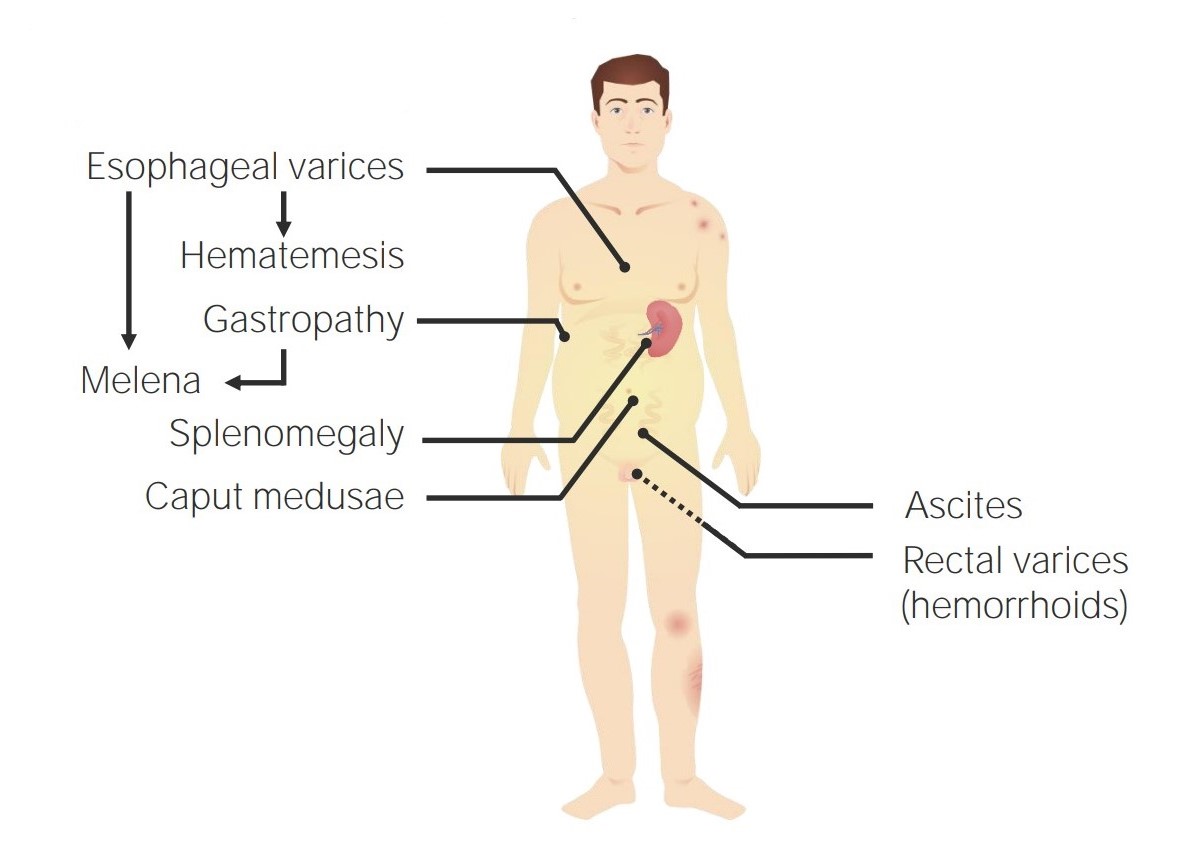
- Blood in stool or black/tarry stools.
- Severe, unrelenting abdominal pain.
- Unexplained weight loss.
- Vomiting or inability to pass gas.
- Sudden change in bowel habits after age 50.
- Nighttime bathroom trips that disturb sleep.
The CDC emphasizes that persistent red-flag symptoms may indicate a more serious underlying condition such as colorectal cancer or a large bowel obstruction.
Where Is Constipation Pain Felt?
Most people report a dull ache in the lower abdomen, often on the left side where the colon stores waste. Some feel pressure near the rectum, especially if stool is hard and stuck. The pain can radiate toward the lower back or hips, making it easy to mistake it for a muscle strain.
Real-World Anecdote
Emma, a 42-year-old teacher, dismissed occasional bloating as just stress. After six months of worsening discomfort, she finally saw a doctor when she noticed blood on toilet paper. Tests revealed a fecal impaction that required gentle manual removal. Emma's story underscores how ignoring subtle danger signs can lead to painful, invasive interventions.
Quick Relief vs. Permanent Fix
Immediate Home Remedies
When the bathroom feels like a distant dream, try these quick-fire steps:
- Drink a glass of warm water with lemon first thing in the morning.
- Add a tablespoon of ground flaxseed to yogurt or oatmeal.
- Take a brisk 10-minute walk after meals to stimulate peristalsis.
- Use an over-the-counter bulk-forming agent like psyllium husk (follow the label).
How to Cure Chronic Constipation PermanentlyStep-by-Step Plan
Short-term fixes help, but lasting relief needs a lifestyle overhaul. Here's a roadmap you can start today:
1. Diet Overhaul
Aim for 25-30 grams of fiber daily. Think berries, apples with skin, lentils, broccoli, and whole-grain breads. If you're not a fan of high-fiber foods, a fiber supplement can bridge the gap.
2. Hydration Schedule
Target 8-10 cups of water spread throughout the day. A good rule: drink a cup every hour you're awake, and sip extra after meals to help fiber do its job.
3. Movement Routine
A daily 30-minute walk, yoga flow, or gentle bike ride gets the intestines moving. Even a short toilet-time stretch (knees to chest while seated) can improve pelvic floor coordination.
4. Behavioral Techniques
Set a regular toilet time after meals when the gastrocolic reflex is strongest. Sit with your feet supported on a footstool to align the rectum and relax the pelvic floor.
5. Medication Review
Talk to your doctor about any drugs that might be slowing you downespecially opioids, anticholinergics, or certain antidepressants. A dosage tweak or a switch to a constipation-friendly alternative can make a big difference.
Incorporating insights from gastroenterologists, this plan addresses both root causes and symptom relief.
Medical Treatment Options Overview
| Option | Who It's For | How It Works | Typical Duration |
|---|---|---|---|
| Bulk-forming agents (psyllium) | Mild-moderate | Adds water to stool, increases bulk | Ongoing |
| Osmotic laxatives (PEG) | Moderate | Draws water into colon | 12 weeks |
| Stimulant laxatives (senna) | Severe | Stimulates intestinal muscle contractions | Short-term |
| Prescription meds (lubiprostone, linaclotide) | Refractory | Enhances fluid secretion in the gut | Long-term |
| Biofeedback therapy | Pelvic-floor dysfunction | Trains pelvic muscles for coordinated evacuation | 6-12 weeks |
Body Effects of Chronic Constipation
Short-Term Discomforts
Beyond the obvious bloating, you might notice nausea, loss of appetite, or a general sense of fullness. These happen because waste sits longer, releasing gases and irritating the gut lining.
Long-Term Complications
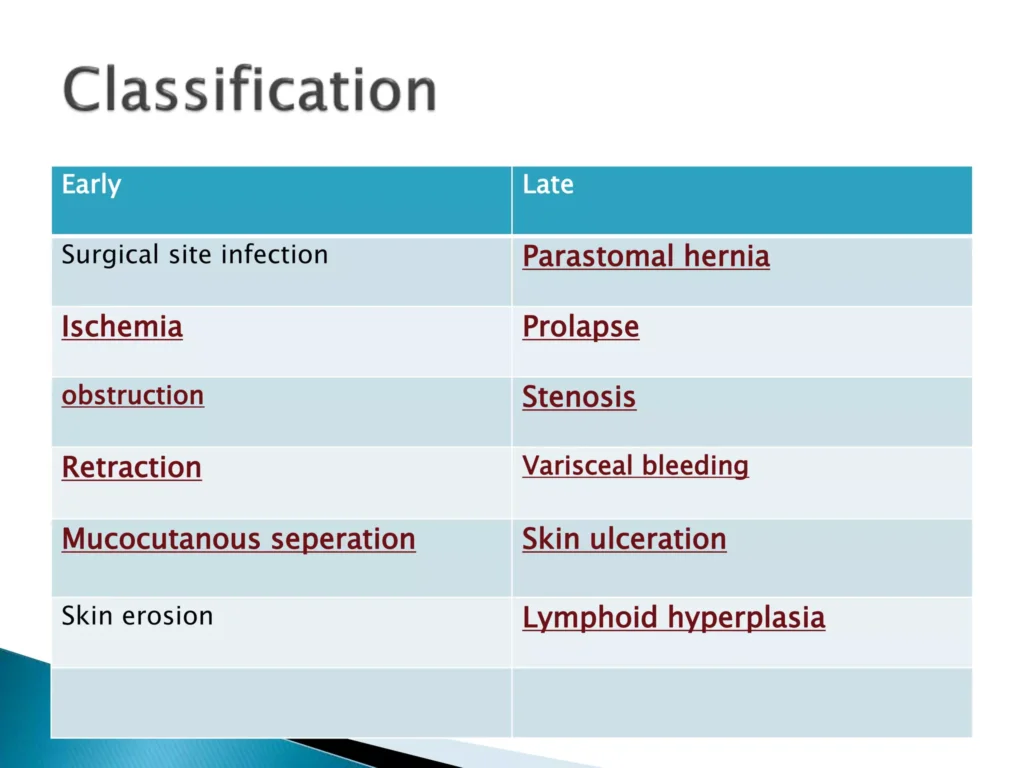
- Fecal impaction: A solid mass of stool that can't be passed without medical help.
- Hemorrhoids & anal fissures: Result from repeated straining.
- Rectal prolapse: The rectum protrudes through the anus after chronic pressure.
- Mental health impact: Ongoing discomfort can fuel anxiety and depression, creating a vicious cycle.
Visual Flowchart (Textual)
Constipation Increased colonic pressure Hemorrhoids / Anal fissures Chronic pain & possible infection Systemic effects (fatigue, mood changes).
Lifestyle Tools & Resources
Tracking Your Bowel Habits
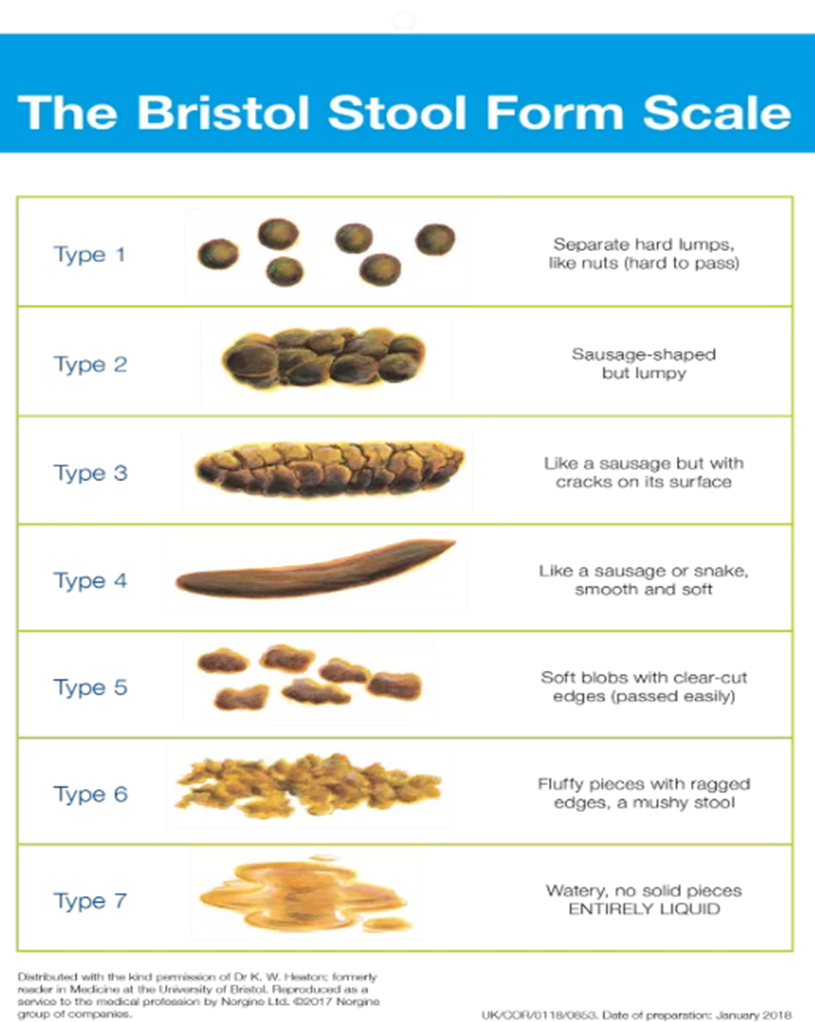
Use a simple printable log or a smartphone app like MyGiHealth to note stool frequency, consistency (the Bristol Stool Chart), and any triggers. Patterns become clearer, and you'll have concrete data to discuss with your physician.
Sample 7-Day High-Fiber Meal Plan
Below is a quick-start menu to boost your fiber intake without feeling like you're chewing cardboard.
| Day | Breakfast | Lunch | Dinner | Snack |
|---|---|---|---|---|
| 1 | Oatmeal with berries & flaxseed | Quinoa salad with chickpeas, veggies | Grilled salmon, roasted broccoli | Apple with almond butter |
| 2 | Greek yogurt, pear, chia seeds | Lentil soup, whole-grain roll | Stir-fried tofu, brown rice, bok choy | Carrot sticks, hummus |
| 3 | Whole-grain toast, avocado, poached egg | Turkey wrap with spinach, whole-wheat tortilla | Spaghetti whole-wheat, tomato basil sauce | Orange slices |
| 4 | Smoothie (kale, banana, oat milk) | Bean burrito bowl, corn, salsa | Baked cod, sweet potato, green beans | Handful of almonds |
| 5 | Millet porridge, dried apricots | Chicken Caesar salad on romaine (light dressing) | Veggie curry, quinoa | Greek yogurt with honey |
| 6 | Scrambled eggs, tomato, whole-grain English muffin | Black-bean soup, side of kale chips | Beef stir-fry, soba noodles | Peach |
| 7 | Chia pudding, mixed berries | Grilled veggie panini, whole-grain bread | Roasted chicken, quinoa pilaf | Celery sticks, peanut butter |
When to Talk to a DoctorDecision Tree
If you answer yes to any of these, schedule an appointment:
- Bleeding or black stools?
- Sudden severe abdominal pain?
- No improvement after 2 weeks of diet & lifestyle changes?
- Weight loss or nighttime bathroom trips?
Bottom LineA Balanced Takeaway
Chronic constipation isn't just an annoying hiccup; it can be a signal that your gut needs more fiber, water, movement, or perhaps a medical review. By recognizing danger signs, tackling the root causes, and applying a blend of everyday habits with evidence-based treatments, you can restore regular, comfortable bowel movements.
If you've tried the basics and still feel stuck, don't hesitate to reach out to a healthcare professional. A tailored planwhether it's a gentle biofeedback session or a prescription medicationcan make all the difference.
Conclusion
Living with chronic constipation is frustrating, but it's also manageable. Understanding why it happens, watching for red-flag symptoms, and committing to a balanced, fiber-rich diet plus regular activity can bring lasting relief. Take the first step today: log your meals, sip that extra glass of water, and schedule a chat with your doctor if the danger signs appear. Your gut will thank you, and you'll reclaim the freedom of feeling light and energized again.
What's your experience with constipation? Have you found a trick that actually works? Share your thoughts in the commentslet's help each other feel better!
FAQs
What are the main lifestyle changes that can help chronic constipation?
Increasing dietary fiber, staying well‑hydrated, adding regular physical activity, and establishing a consistent toileting routine are the most effective lifestyle adjustments.
When should I see a doctor for chronic constipation?
Seek medical attention if you notice blood in stool, severe abdominal pain, sudden changes after age 50, weight loss, or if symptoms persist despite 2 weeks of diet and lifestyle modifications.
Are there any over‑the‑counter medications that work for chronic constipation?
Bulk‑forming agents like psyllium, osmotic laxatives such as polyethylene glycol (PEG), and stimulant laxatives like senna can provide relief, but they should be used as directed and discussed with a healthcare professional.
How does chronic constipation affect mental health?
Ongoing discomfort can increase stress, anxiety, and depressive symptoms, creating a cycle where emotional distress further worsens bowel function.
What is the ICD‑10 code for chronic constipation?
The ICD‑10 code for chronic constipation is K59.0, which clinicians use to document the condition and any related underlying diseases.