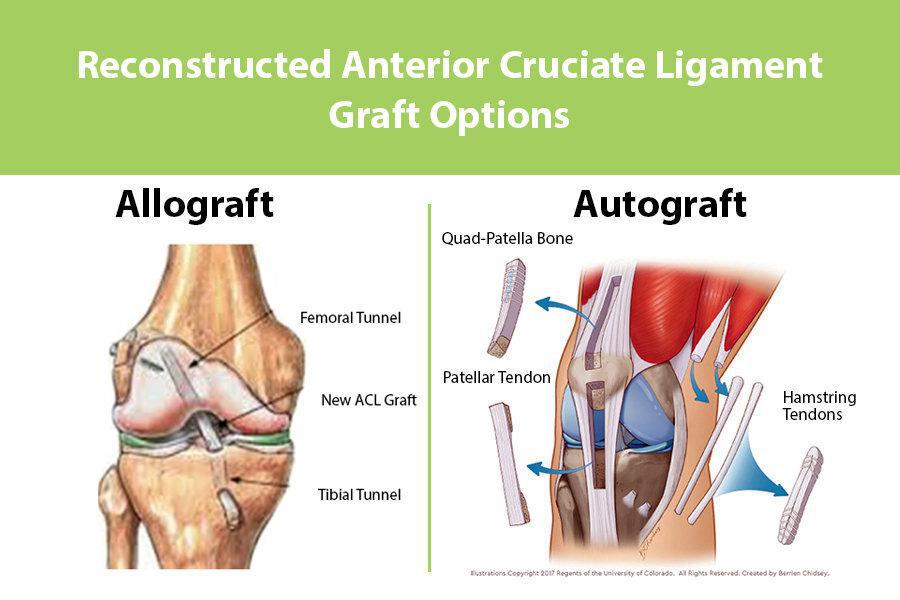
Did you know that the choice between an allograft and an autograft can feel a lot like picking the right pair of shoes for a marathon? One option uses your own tissue, the other borrows from a donor, and each has its own comfort level, fit, and recovery timeline. In this guide Ill walk you through the essentials, share realworld stories, and help you decide which graft might be the right match for you.
What Is Autograft?
An autograft means selfgraft. In plain English, its tissue taken from somewhere else in your own body and moved to the site that needs repair. Think of it like using a piece of your own fabric to patch a tear in a favorite shirt it fits perfectly because its the same material.
Typical Sources
- Hamstring tendon (semitendinosus or gracilis)
- Patellartendon (bonepatellartendonbone, BPTB)
- Iliac crest bone for spinal fusions
- Skin grafts for burns or wounds
How Its Harvested
The surgeon makes a small incision at the donor site, carefully removes the chosen tissue, and then stitches the area closed. The graft is then shaped and placed where its needed for example, inside the knee during an ACL reconstruction. The whole process adds a bit of extra surgical time, but the tissue is yours, so the body recognises it immediately.
Pros of Autograft
- Highest biological compatibility no risk of immune rejection.
- Faster incorporation: the graft typically locks in within 36months.
- Lower risk of disease transmission (because its your own tissue).
Cons of Autograft
- Donorsite pain youll feel soreness where the tissue was taken.
- Limited quantity you cant harvest endless amounts.
- Longer operative time and a second incision.
According to a recent metaanalysis published in , patients who received autografts reported higher rates of early return to sport compared with allograft recipients, largely because the body integrates the tissue more quickly.
What Is Allograft?
An allograft comes from a donor usually a cadaveric donor whose tissue has been screened, processed, and stored in a certified tissue bank. Think of it as borrowing a spare tire from a neighbour; it fits the car, but you have to make sure its been inspected and cleaned first.
Where It Comes From
Allografts are sourced from accredited tissue banks that follow strict FDA and AATB (American Association of Tissue Banks) standards. Donor tissue is screened for infectious diseases, sterilised (often with lowdose radiation), and cryopreserved or freezedried to keep it viable.
Types of Allograft Tissue
- Bone (cortical, cancellous, or bulk structural)
- Tendon (Achilles, hamstring, tibialis anterior)
- Skin (used for burns or large wounds)
- Meniscus and ligament tissue for knee repairs
Pros of Allograft
- No second incision you avoid donorsite pain.
- Unlimited supply perfect for large defects or revision surgeries.
- Shorter operative time because the graft is ready to go.
Cons of Allograft
- Slower incorporation it can take 612months for full biologic integration.
- Small risk of disease transmission (less than 0.01% when properly screened).
- Potentially lower initial biomechanical strength compared with autograft.
The notes that modern processing methods have dramatically reduced infection risk, making allografts a safe choice for many patients.
Allograft vs Autograft Comparison
| Feature | Autograft | Allograft |
|---|---|---|
| Source | Your own tissue | Donor tissue from a screened bank |
| Healing time | 36months (fast) | 612months (slower) |
| Donorsite morbidity | Yes extra incision pain | No |
| Availability | Limited by anatomy | Unlimited, especially for large defects |
| Disease transmission risk | None | Very low (<0.01%) |
| Typical cost | Lower graft material, higher OR time | Higher graft price, lower OR time |
| Best for | Younger athletes, primary reconstructions | Revision surgery, older patients, large bone defects |
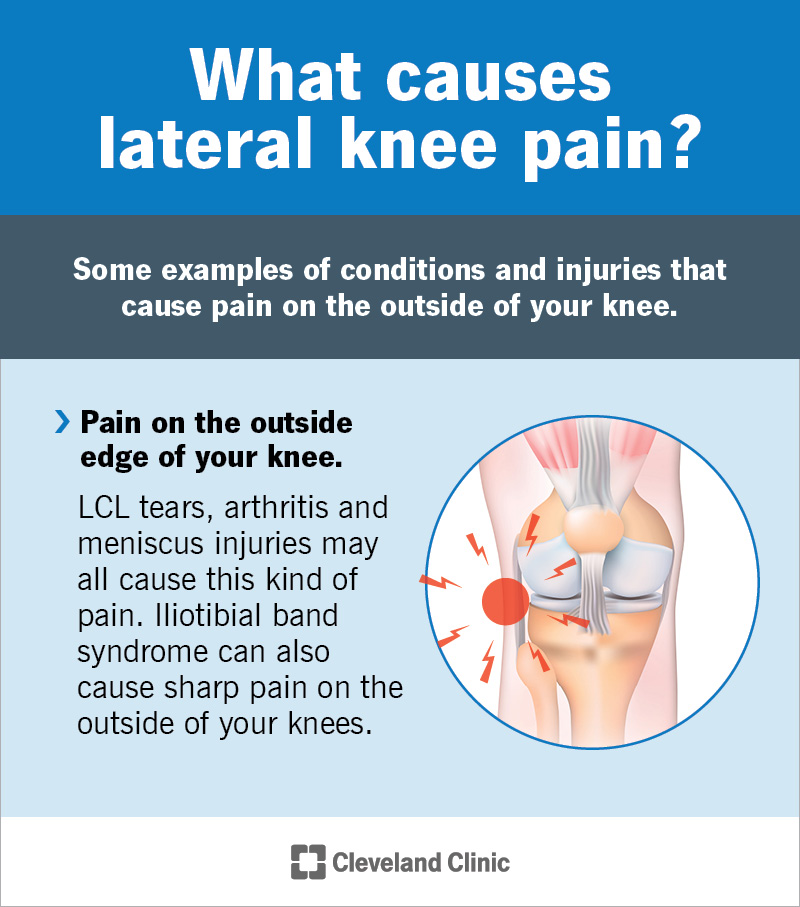
When Is Autograft Preferred for ACL Reconstruction?
If youre a highschool or college athlete dreaming of hitting the field again within a year, many surgeons lean toward an autograft because the graft integrates quickly and offers robust initial strength. Studies in the American Journal of Sports Medicine show a lower retear rate for hamstring autografts in patients under 30.
When Is Allograft the Goto Choice?
For a 55yearold whos getting a knee revision or a spinal fusion, the extra incision from an autograft may not be worth the tradeoff. Allografts let the surgeon avoid donorsite pain and keep the operation shorter a big plus when recovery time is already a concern. In spinal fusion cases, combining autograft bone with an allograft scaffold is common to balance osteogenic potential with volume needs; this approach links to considerations similar to those discussed in osteoporosis physical therapy when optimizing bone health and rehab after surgery.
Key Specialty Applications
ACL Reconstruction
Both graft types are FDAapproved for ACL repair, but the decision hinges on age, activity level, and surgeon experience. Autograft (hamstring or patellartendon) typically offers quicker returntosport, while allograft can be advantageous for multiligament injuries where you need multiple grafts.
Spinal Fusion & Bone Grafting
When fusing vertebrae, surgeons may use a blend of autograft bone from the iliac crest and allograft bone chips. The autograft provides osteogenic cells, while the allograft supplies a scaffold.
SoftTissue & Skin Grafts
In burn care, an allograft skin can act as a temporary biological dressing while your own skin heals. This is different from an autograft, which would require harvesting skin from an unburned area something you usually want to avoid if possible.
Other Comparisons
- Allograft vs Xenograft: Xenografts come from a different species (often porcine or bovine) and are rarely used in orthopedics due to higher immunogenicity.
- Autograft vs Allograft vs Homograft: Homograft is another term for allograft; the distinction is mostly historical.
- Isograft vs Allograft: An isograft is tissue from an identical twin extremely rare outside of research.
- Allograft vs Autograft vs Synthetic: Synthetic grafts (e.g., LARS ligament) are still experimental for many indications and generally reserved for specific cases where biological grafts arent feasible.
How To Decide
Choosing a graft isnt a onesizefitsall decision. Below are the key factors you should weigh, ideally together with your surgeon during the preoperative consultation.
Age & Activity Level
Young, highimpact athletes often benefit from the rapid healing of an autograft. Older or less active patients may prioritize a lowerpain option, making an allograft attractive.
Size & Location of the Defect
If the area needing repair is large (think multiligament knee injury or a massive bone loss), the limited supply of autograft tissue could be a showstopper. Allografts fill that gap.
Medical History
Conditions like diabetes, smoking, or poor vascular supply can slow healing. Some surgeons prefer an allograft in smokers to avoid donorsite complications, while others argue that an autografts innate biology may still outperform a donor graft in compromised patients.
Surgeon Experience
Never underestimate the importance of whos performing the surgery. A surgeon who has done thousands of autograft ACL reconstructions will have refined techniques that reduce donorsite morbidity. Conversely, a specialist in complex revisions may have a strong track record with allografts.
Insurance & Cost
Insurance plans often differentiate between graft types. Autograft material itself is free, but the added operative time can affect overall cost. Allografts carry a procurement fee that can be significant. Its worth asking your provider for a cost breakdown before you sign any consent forms.
Decision Checklist
- Write down your primary goal (return to sport, pain relief, etc.).
- List any health concerns that might affect healing.
- Ask your surgeon about their experience with each graft type.
- Verify insurance coverage for both options.
- Consider a second opinion if youre uncertain.
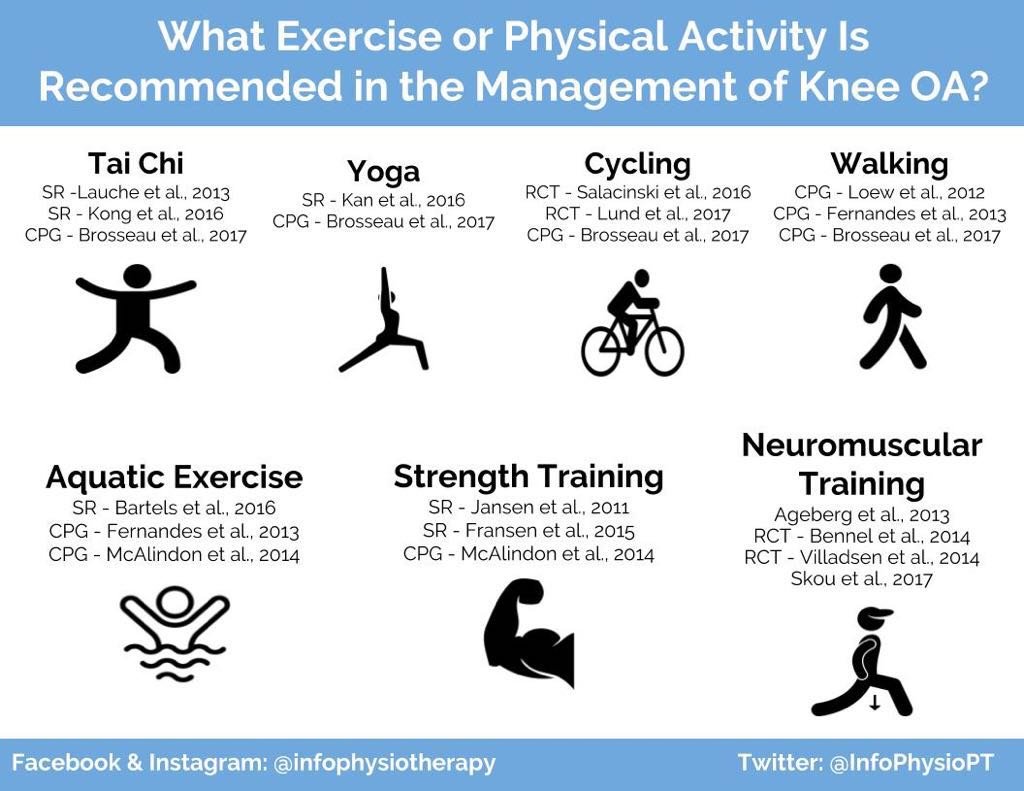
Recovery and Rehabilitation
Regardless of graft choice, rehab is the bridge between surgery and the life you want to get back to. Heres a rough timeline you can expect, but remember that individual progress varies.
Weeks 02: Immediate PostOp
Both grafts require protected weightbearing, crutches, and a knee brace set to limit flexion. Youll feel soreness at the surgical site and, if you had an autograft, at the donor site (often the hamstring or patellartendon area).
Weeks 26: Early Mobility
Physical therapy focuses on range of motion, gentle quad activation, and controlled walking. Autograft patients often notice faster reduction in swelling, while allograft patients may need a bit more patience as the graft settles in.
Weeks 612: Strength Building
This is where the differences become more evident. Autograft recipients may start light jogging and sportspecific drills earlier, whereas allograft patients might stay on a bike or elliptical a little longer. However, modern allograft processing has narrowed this gap considerably.
Months 36: Return to Sport
Most surgeons clear patients for full activities after 69months, depending on functional testing. Autograft patients often hit the 6month mark, but allograft patients who followed a disciplined rehab can be just as ready by nine months.
Tips to Accelerate Healing
- Maintain a proteinrich diet think lean meats, beans, and dairy.
- Stay hydrated; water aids cellular repair.
- Avoid smoking nicotine constricts blood vessels.
- Follow your therapists progression schedule; dont rush.
- Consider lowimpact crosstraining (swimming, cycling) to keep cardiovascular fitness without stressing the joint.
Final Takeaways & Action
Both allograft and autograft have their own set of strengths and tradeoffs. Autografts give you the fastest biological integration but come with a second incision and donorsite discomfort. Allografts spare you that extra cut and provide an abundant supply, though they may need a bit more time to fully incorporate.
The right choice is personal it depends on your age, activity goals, medical background, and even your insurance plan. The most empowering step you can take right now is to write down your priorities, bring those notes into your preop visit, and ask your surgeon specific questions about their experience with each graft type. By doing that, youll turn a complex medical decision into a clear, confidencebuilding conversation.
Whats your experience with grafts? Have you or a loved one gone through an ACL repair, spinal fusion, or burn reconstruction? Share your story in the comments your insight could help someone else make a more informed choice. And if you have any lingering questions, feel free to ask Im here to help you navigate this journey.
FAQs
What is the main difference between an allograft and an autograft?
An autograft uses tissue taken from your own body, while an allograft comes from a screened donor and is processed before implantation.
Which graft type is preferred for young athletes undergoing ACL reconstruction?
Most surgeons recommend an autograft for younger, high‑activity athletes because it integrates faster and provides stronger initial biomechanical stability.
Is there a risk of disease transmission with allografts?
When properly screened and processed, the risk is extremely low—generally less than 0.01 %—but it is not zero.
How does donor‑site pain impact recovery after an autograft?
Donor‑site pain is common after autograft harvest and can prolong early rehabilitation, especially if the hamstring or patellar tendon is taken.
What factors should I consider when choosing between allograft and autograft?
Consider your age, activity level, size of the defect, medical history, surgeon’s experience, and insurance coverage to determine the best option for your recovery.